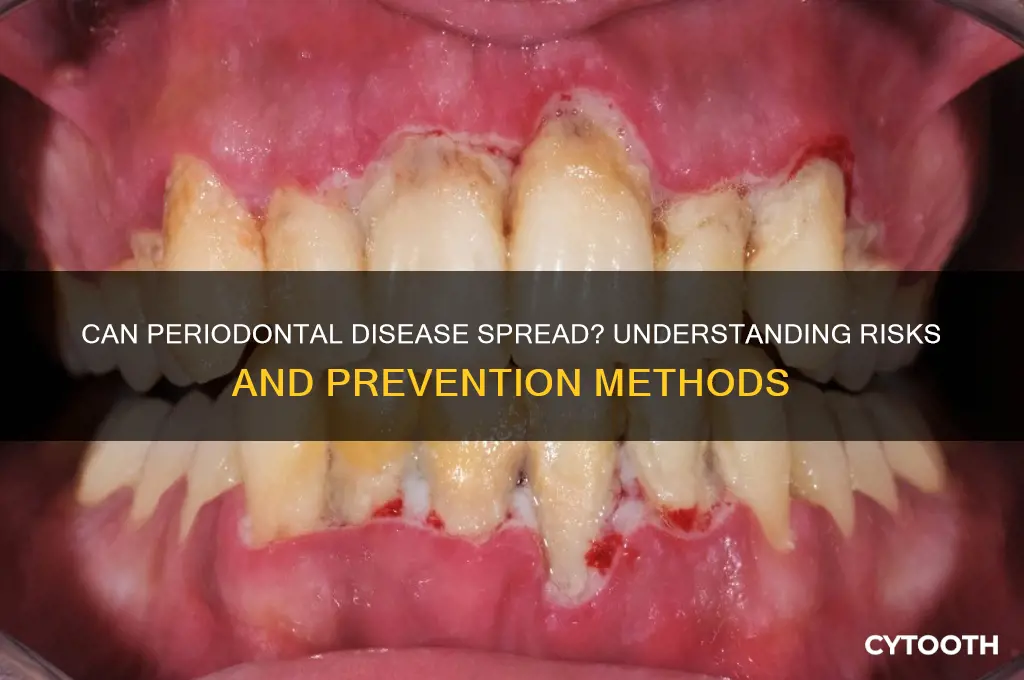
Periodontal disease, a chronic inflammatory condition affecting the gums and supporting structures of the teeth, raises concerns about its potential to spread beyond the oral cavity. While primarily localized to the mouth, research suggests that the bacteria and inflammatory markers associated with periodontal disease can enter the bloodstream, potentially contributing to systemic health issues. Conditions such as cardiovascular disease, diabetes, and respiratory infections have been linked to periodontal pathogens, indicating that the disease may not remain isolated. Additionally, the spread of periodontal bacteria to adjacent teeth or tissues can exacerbate local damage, leading to progressive bone loss and tooth mobility. Understanding the mechanisms by which periodontal disease may spread is crucial for developing comprehensive treatment strategies and preventing its broader health implications.
| Characteristics | Values |
|---|---|
| Can Periodontal Disease Spread? | Yes, periodontal disease can spread from one person to another, primarily through direct contact with saliva or infected materials. |
| Mode of Transmission | Bacterial transfer via kissing, sharing utensils, or toothbrushes. The primary bacteria involved are Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans. |
| Risk Factors for Spread | Close personal contact, poor oral hygiene, compromised immune system, and genetic predisposition. |
| Spread Within the Mouth | Periodontal disease can spread from one tooth to another within the same individual due to bacterial migration and inflammation. |
| Systemic Spread | Bacteria from periodontal disease can enter the bloodstream, potentially affecting other parts of the body, such as the heart, lungs, and exacerbating conditions like diabetes. |
| Prevention of Spread | Maintaining good oral hygiene, regular dental check-ups, avoiding sharing personal items, and early treatment of gum disease. |
| Treatment to Prevent Spread | Scaling and root planing, antibiotic therapy, and surgical interventions to remove infected tissue. |
| Public Health Impact | Periodontal disease is a significant public health concern due to its prevalence and potential for spread, emphasizing the need for community-based oral health programs. |
What You'll Learn
- Transmission via saliva: Can periodontal bacteria spread through saliva exchange, like kissing or sharing utensils
- Systemic spread: Does periodontal disease contribute to systemic conditions like heart disease or diabetes
- Mother-to-child transmission: Can periodontal pathogens be passed from mother to child during pregnancy or birth
- Household spread: Is periodontal disease contagious among family members living in close proximity
- Dental procedures risk: Can periodontal bacteria spread during dental treatments or via contaminated instruments

Transmission via saliva: Can periodontal bacteria spread through saliva exchange, like kissing or sharing utensils?
Periodontal disease, characterized by inflammation and infection of the gums and supporting structures of the teeth, is primarily caused by bacterial buildup. Among the culprits are species like *Porphyromonas gingivalis* and *Treponema denticola*, which thrive in the oral biofilm. A pressing question arises: can these pathogens be transmitted through saliva exchange, such as during kissing or sharing utensils? Understanding this risk is crucial, as it intersects with everyday behaviors and public health implications.
Saliva serves as a natural reservoir for oral bacteria, including those associated with periodontal disease. Studies have shown that intimate contact, like kissing, can transfer up to 80 million bacteria in a single 10-second exchange. While this may sound alarming, the human body is equipped with defense mechanisms, such as saliva’s antimicrobial properties, which often neutralize harmful invaders. However, individuals with compromised immune systems or poor oral hygiene are more susceptible to colonization by foreign bacteria. Sharing utensils, though less intimate, still poses a risk, particularly if the recipient has open sores or cuts in the mouth, which provide direct entry points for pathogens.
From a practical standpoint, reducing transmission risk involves simple yet effective measures. For instance, maintaining good oral hygiene—brushing twice daily, flossing, and using antimicrobial mouthwash—can significantly lower bacterial load in saliva. For couples, regular dental check-ups and periodontal screenings are advisable, especially if one partner has active gum disease. Parents should avoid sharing spoons or blowing on food for infants, as this can introduce adult oral bacteria into the child’s mouth, potentially disrupting their developing oral microbiome.
Comparatively, while saliva exchange can transmit periodontal bacteria, it is not the primary mode of spread. Chronic periodontal disease is largely driven by personal factors like smoking, diabetes, and genetic predisposition. However, in close relationships, the cumulative effect of repeated bacterial exposure cannot be ignored. For example, a 2019 study published in *Community Dentistry and Oral Epidemiology* found that spouses of individuals with severe periodontitis were 3.7 times more likely to develop the condition themselves. This highlights the importance of shared oral health responsibility in households.
In conclusion, while periodontal bacteria can indeed spread through saliva exchange, the risk is context-dependent. Healthy individuals with robust oral hygiene practices are less likely to experience adverse effects. However, for those with underlying vulnerabilities, even casual contact like sharing a fork or a kiss could serve as a vector for infection. Awareness and proactive measures are key to mitigating this risk, ensuring that intimate moments remain safe and healthy for all involved.
Cost of Gum Disease Treatment: What to Expect and Budget For
You may want to see also

Systemic spread: Does periodontal disease contribute to systemic conditions like heart disease or diabetes?
Periodontal disease, a chronic inflammatory condition affecting the gums and bone supporting the teeth, has long been recognized for its oral health implications. However, emerging research suggests its impact may extend far beyond the mouth. The question arises: Can periodontal disease contribute to systemic conditions such as heart disease or diabetes? Understanding this potential link is crucial, as it could reshape preventive healthcare strategies.
Consider the biological mechanisms at play. Periodontal disease involves the proliferation of harmful bacteria and the release of inflammatory mediators, which can enter the bloodstream. These systemic inflammatory markers, such as C-reactive protein (CRP), have been associated with cardiovascular events. For instance, studies show that individuals with severe periodontitis have a 20-30% higher risk of developing coronary artery disease. Similarly, the chronic inflammation from periodontal disease may exacerbate insulin resistance, a key factor in type 2 diabetes. A 2018 meta-analysis revealed that treating periodontitis improved glycemic control in diabetic patients, as measured by a reduction in HbA1c levels by an average of 0.4%.
From a practical standpoint, addressing periodontal disease could be a preventive measure for systemic health. For adults over 40, routine dental check-ups every six months are essential, especially for those with pre-existing conditions like hypertension or prediabetes. Dentists may recommend deep cleaning procedures, such as scaling and root planing, to reduce bacterial load. Additionally, maintaining oral hygiene at home—brushing twice daily with fluoride toothpaste and flossing daily—can mitigate risks. For diabetic patients, monitoring blood sugar levels is critical, as uncontrolled glucose can worsen periodontal outcomes, creating a bidirectional relationship.
While the evidence is compelling, it’s important to approach the connection cautiously. Not all individuals with periodontal disease will develop systemic conditions, and other factors like genetics, diet, and lifestyle play significant roles. However, the potential for periodontal health to influence overall well-being underscores the need for interdisciplinary care. Collaboration between dentists and primary care physicians could lead to more holistic treatment plans, particularly for at-risk populations.
In conclusion, the systemic spread of periodontal disease’s effects is a growing area of interest. While definitive causality remains under investigation, the existing data strongly suggest a correlation with conditions like heart disease and diabetes. Proactive oral care, combined with awareness of these links, could be a powerful tool in preventing broader health complications. As research evolves, staying informed and taking preventive steps remains the best course of action.
Effective Home Remedies to Treat Gum Disease Without Dental Visits
You may want to see also

Mother-to-child transmission: Can periodontal pathogens be passed from mother to child during pregnancy or birth?
Periodontal disease, a chronic inflammatory condition affecting the gums and bone supporting the teeth, has long been associated with systemic health issues. But can the pathogens responsible for this disease be transmitted from mother to child during pregnancy or childbirth? Emerging research suggests that this vertical transmission is not only possible but may also have significant implications for the child’s future oral and overall health. Studies have identified periodontal pathogens, such as *Porphyromonas gingivalis* and *Aggregatibacter actinomycetemcomitans*, in the placenta and amniotic fluid of pregnant women with periodontitis, raising concerns about their potential to cross the maternal-fetal barrier.
The mechanism of transmission is thought to involve hematogenous spread, where bacteria or their byproducts enter the bloodstream and travel to the placenta. This process can trigger inflammatory responses, potentially contributing to adverse pregnancy outcomes like preterm birth or low birth weight. For instance, a 2018 study published in *Journal of Clinical Periodontology* found that pregnant women with untreated periodontitis had a higher risk of preterm birth, with periodontal pathogens detected in the placenta of affected cases. While the direct causation remains under investigation, these findings underscore the importance of maternal oral health during pregnancy.
Preventing mother-to-child transmission of periodontal pathogens begins with proactive dental care. Pregnant women should prioritize regular dental check-ups, ideally in the second trimester when risk of complications is lower. Non-surgical periodontal therapy, such as scaling and root planing, can effectively reduce bacterial load without posing risks to the fetus. Additionally, maintaining good oral hygiene at home—brushing twice daily with fluoride toothpaste, flossing daily, and using antimicrobial mouthwash—can minimize pathogen levels. For women with severe periodontitis, consultation with both a dentist and obstetrician is crucial to tailor treatment plans that balance maternal and fetal safety.
Comparatively, the risk of transmission is not limited to pregnancy; it extends to postnatal interactions, particularly during breastfeeding. Periodontal pathogens can be present in saliva, and close contact between mother and child may facilitate bacterial transfer. While the long-term effects of this exposure are still being studied, early colonization of a child’s oral cavity by these pathogens could predispose them to future periodontal issues. To mitigate this, mothers should avoid sharing utensils or cleaning pacifiers with their mouths, and ensure their children receive proper oral care as soon as the first tooth erupts.
In conclusion, while the evidence of mother-to-child transmission of periodontal pathogens is compelling, it is not a reason for alarm but rather a call to action. By integrating oral health into prenatal care and adopting preventive measures, mothers can significantly reduce the risk of passing these pathogens to their children. As research continues to unravel the complexities of this transmission, one thing is clear: a healthy mouth is a critical component of a healthy pregnancy and a healthy start for the next generation.
Recognizing Gum Disease: Symptoms, Appearance, and Early Warning Signs
You may want to see also

Household spread: Is periodontal disease contagious among family members living in close proximity?
Periodontal disease, a chronic inflammatory condition affecting the gums and bone supporting the teeth, is primarily caused by bacterial plaque buildup. While it is not contagious in the traditional sense, like a cold or flu, the bacteria responsible for the disease can be transmitted through saliva. This raises a critical question for families: Can living in close proximity increase the risk of one family member’s periodontal disease affecting others? Understanding this dynamic is essential for households aiming to maintain oral health collectively.
The transmission of periodontal pathogens, such as *Porphyromonas gingivalis* and *Treponema denticola*, typically occurs through direct contact with saliva. Sharing utensils, toothbrushes, or even kissing can facilitate the spread of these bacteria. In households where family members share meals, personal items, or engage in close physical contact, the risk of bacterial transfer is heightened. For instance, a study published in the *Journal of Clinical Periodontology* found that spouses of individuals with severe periodontitis had a 50% higher likelihood of developing the condition themselves. This suggests that proximity and shared habits play a significant role in bacterial transmission.
Preventing household spread requires proactive measures. First, avoid sharing personal items like toothbrushes, drinking glasses, or eating utensils. Encourage family members to maintain good oral hygiene practices, including brushing twice daily with fluoride toothpaste and flossing regularly. For children under 12, supervise brushing to ensure proper technique and prevent accidental sharing of toothbrushes. Additionally, consider using antimicrobial mouthwashes to reduce bacterial load in the mouth, especially if one family member is already diagnosed with periodontal disease.
Age and immune status are critical factors in household spread. Older adults and individuals with compromised immune systems are more susceptible to periodontal disease and its complications. If a family member falls into these categories, extra precautions are necessary. For example, ensure separate kitchenware and maintain a clean living environment to minimize bacterial exposure. Regular dental check-ups for all family members are also vital, as early detection and treatment can prevent the progression of the disease and reduce the risk of transmission.
In conclusion, while periodontal disease is not directly contagious, the bacteria causing it can spread through close contact in household settings. By adopting simple yet effective preventive measures, families can significantly reduce the risk of transmission. Awareness, hygiene, and regular dental care are key to safeguarding oral health for everyone under one roof.
Gum Disease Treatment Costs: What to Expect and How to Budget
You may want to see also

Dental procedures risk: Can periodontal bacteria spread during dental treatments or via contaminated instruments?
Periodontal disease, characterized by inflammation and infection of the gums and supporting structures of the teeth, is primarily caused by bacterial biofilms. These bacteria, if left unchecked, can lead to systemic health issues, including cardiovascular disease and diabetes. A critical concern arises when considering whether these pathogens can spread during dental procedures or via contaminated instruments. The risk is not hypothetical; it is a documented reality that demands attention from both dental professionals and patients.
Steps to Minimize Bacterial Spread During Dental Procedures
Dental treatments, such as scaling and root planing, inherently disturb bacterial biofilms, releasing pathogens into the oral cavity and potentially the bloodstream. To mitigate this, dentists follow strict infection control protocols. Instruments must be sterilized using autoclaves at temperatures of 121°C (250°F) for at least 15 minutes, ensuring the elimination of all microorganisms, including periodontal bacteria. Additionally, single-use items, such as gloves and suction tips, should never be reused. Patients can advocate for their safety by inquiring about a clinic’s sterilization practices before treatment.
Cautions for High-Risk Individuals
Immunocompromised patients, the elderly, and those with pre-existing conditions face heightened risks if exposed to periodontal bacteria during dental procedures. For instance, bacteremia—the presence of bacteria in the bloodstream—can occur post-treatment, potentially leading to endocarditis or joint infections in susceptible individuals. Dentists should take extra precautions, such as prescribing prophylactic antibiotics for at-risk patients, particularly before invasive procedures like extractions or implant placements.
Comparative Analysis of Contamination Risks
While modern dental practices prioritize sterilization, lapses can occur. A 2015 study published in the *Journal of Dental Research* found that 10% of dental instruments tested positive for bacterial contamination post-sterilization, primarily due to inadequate cleaning before autoclaving. In contrast, clinics using ultrasonic cleaners and enzymatic detergents prior to sterilization reported significantly lower contamination rates. This highlights the importance of a multi-step disinfection process, not just reliance on autoclaves.
Practical Tips for Patients
Patients can reduce their risk by choosing dental providers who adhere to CDC guidelines for infection control. Observing the clinic’s hygiene practices, such as the use of barrier protection on equipment and proper disposal of single-use items, is essential. Post-treatment, maintaining oral hygiene with antimicrobial mouthwashes can help eliminate any residual bacteria. For those with periodontal disease, regular follow-ups and early intervention are key to preventing bacterial spread during future procedures.
In conclusion, while dental treatments carry an inherent risk of spreading periodontal bacteria, adherence to rigorous sterilization protocols and patient vigilance can significantly minimize this threat. Both dentists and patients play critical roles in ensuring a safe treatment environment.
Effective Toothpaste Options to Reverse Gum Disease and Restore Oral Health
You may want to see also
Frequently asked questions
No, periodontal disease is not contagious and cannot spread directly from one person to another. It is caused by bacterial buildup in the mouth, not by a virus or bacteria that can be transmitted through contact.
Yes, periodontal disease can spread from one tooth to another if left untreated. The bacteria causing the infection can migrate to adjacent teeth and gums, worsening the condition over time.
Yes, untreated periodontal disease can lead to systemic health issues. The bacteria and inflammation associated with it can enter the bloodstream, potentially affecting the heart, lungs, and other organs.
While periodontal disease primarily affects the gums and teeth, the bacteria causing it can contribute to other oral infections, such as thrush or tonsillitis, if oral hygiene is poor.
No, periodontal disease itself cannot spread through kissing or sharing utensils. However, the bacteria causing it can be transferred, though this does not guarantee the other person will develop the disease.