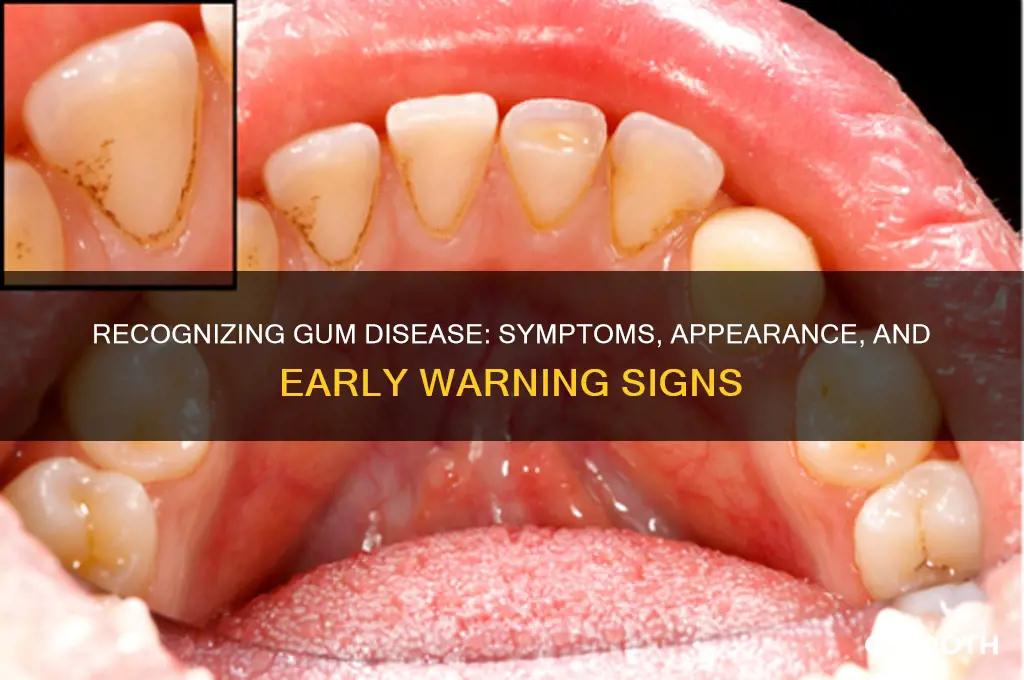
Gum disease, also known as periodontal disease, often begins subtly but can progress to cause significant oral health issues if left untreated. Early signs include red, swollen, or tender gums that may bleed during brushing or flossing, a condition known as gingivitis. As the disease advances, symptoms can worsen, leading to receding gums, persistent bad breath, and the formation of pockets between the teeth and gums where bacteria accumulate. In severe cases, known as periodontitis, teeth may become loose or shift, and bone loss can occur, potentially resulting in tooth loss. Recognizing these visual and physical indicators early is crucial for timely intervention and prevention of long-term damage.
What You'll Learn
- Red, swollen gums: Inflammation and redness are early signs of gingivitis, the initial stage of gum disease
- Bleeding gums: Gums that bleed easily during brushing or flossing indicate gum irritation or infection
- Receding gums: Gums pulling away from teeth expose roots, a common symptom of advanced gum disease
- Persistent bad breath: Halitosis can result from bacteria buildup and infection in the gums and teeth
- Loose or shifting teeth: Advanced gum disease damages bone support, causing teeth to feel loose or move

Red, swollen gums: Inflammation and redness are early signs of gingivitis, the initial stage of gum disease
Red, swollen gums are often the first visible warning signs of gingivitis, the earliest stage of gum disease. This inflammation occurs when bacteria in plaque build up along the gum line, triggering an immune response. The gums react by becoming puffy, tender, and bright red—a stark contrast to their normal pale pink, firm appearance. If you notice these symptoms, especially after brushing or flossing, it’s a clear signal that your oral hygiene routine needs attention. Ignoring these early signs can allow the condition to progress into more severe forms of gum disease, such as periodontitis, which can lead to tooth loss and other systemic health issues.
To address red, swollen gums effectively, start by evaluating your oral care habits. Brush your teeth twice daily with a soft-bristled toothbrush and fluoride toothpaste, ensuring you clean along the gum line where plaque accumulates. Floss daily to remove debris between teeth, and consider using an antimicrobial mouthwash to reduce bacterial growth. For adults, a 0.12% chlorhexidine mouthwash, used twice daily for 30 seconds each time, can help control inflammation. However, consult your dentist before starting any new oral care product, especially if you’re pregnant, nursing, or have children under 12, as some products may not be suitable.
Comparatively, while red, swollen gums are a common issue, they can sometimes be mistaken for other conditions, such as oral allergies or fungal infections. Allergic reactions often cause itching or hives, whereas fungal infections like thrush present as white patches in the mouth. Gingivitis, however, is characterized specifically by localized redness and swelling along the gum line. If you’re unsure about the cause of your symptoms, a dental professional can provide a definitive diagnosis and recommend appropriate treatment. Early intervention is key—gingivitis is reversible with proper care, but delaying treatment increases the risk of irreversible damage.
Practically, incorporating anti-inflammatory foods into your diet can support gum health alongside improved oral hygiene. Foods rich in vitamin C, such as oranges, strawberries, and bell peppers, help reduce inflammation and strengthen gum tissue. Omega-3 fatty acids, found in fish like salmon and flaxseeds, also have anti-inflammatory properties. Avoid sugary snacks and beverages, as they fuel bacterial growth and exacerbate inflammation. Finally, schedule regular dental check-ups every six months for professional cleanings and early detection of any issues. By taking these steps, you can address red, swollen gums proactively and prevent the progression of gum disease.
Understanding the Timeline: How Long Does Gum Disease Develop?
You may want to see also

Bleeding gums: Gums that bleed easily during brushing or flossing indicate gum irritation or infection
Bleeding gums are often one of the first signs of gum disease, a condition that can escalate from mild irritation to severe infection if left untreated. When you notice blood on your toothbrush or in the sink after flossing, it’s your body’s alarm system signaling that something is wrong. This symptom typically arises from the inflammation of gum tissue, known as gingivitis, which occurs when plaque builds up along the gum line. Ignoring this warning can lead to more serious issues, such as periodontitis, where the infection spreads deeper into the gum tissue and bone, potentially causing tooth loss.
To address bleeding gums effectively, start by evaluating your oral hygiene routine. Brush your teeth twice daily with a soft-bristled toothbrush, using gentle, circular motions to avoid further irritation. Floss daily to remove plaque and food particles between teeth, but be cautious not to snap the floss into the gums, as this can worsen bleeding. Incorporate an antimicrobial mouthwash into your routine to reduce bacterial growth and soothe inflamed gums. If bleeding persists after two weeks of consistent care, consult a dentist, as this may indicate a more advanced stage of gum disease requiring professional intervention.
Comparing bleeding gums to other oral health issues highlights their role as an early warning sign. Unlike tooth sensitivity or bad breath, which can stem from various causes, bleeding gums are almost always linked to gum inflammation or infection. For instance, while tooth sensitivity might result from enamel erosion or exposed roots, bleeding gums specifically point to issues at the gum line. Recognizing this distinction can help you take targeted action before the problem progresses.
Practically speaking, preventing bleeding gums involves more than just brushing and flossing. Limit sugary and acidic foods, which contribute to plaque formation, and stay hydrated to maintain saliva production, your mouth’s natural defense against bacteria. For adults over 40, regular dental check-ups are crucial, as gum disease risk increases with age. If you’re pregnant, be especially vigilant, as hormonal changes can make gums more susceptible to inflammation. By combining these habits with prompt attention to bleeding, you can protect your gums and overall oral health.
Reversing Periodontal Gum Disease: Is It Possible and How?
You may want to see also

Receding gums: Gums pulling away from teeth expose roots, a common symptom of advanced gum disease
Receding gums, a telltale sign of advanced gum disease, manifest as the gum tissue pulls away from the teeth, exposing the sensitive roots beneath. This condition, known as gingival recession, not only alters the appearance of your smile but also compromises oral health. Visually, you might notice your teeth appear longer than before, or you may see a notch-like gap where the gum meets the tooth. If left untreated, this exposure can lead to increased tooth sensitivity, decay, and even tooth loss.
To identify receding gums, examine your teeth in a mirror, looking for areas where the gum line seems lower than usual or where the tooth root is visible. Another indicator is persistent sensitivity to hot, cold, or sweet stimuli, as the protective gum layer is no longer shielding the nerve-rich dentin. If you suspect recession, it’s crucial to consult a dentist promptly. Early intervention can prevent further damage and may include deep cleaning (scaling and root planing) to remove plaque and tartar buildup, a primary cause of gum disease.
Preventing gum recession starts with diligent oral hygiene. Brush twice daily with a soft-bristled toothbrush, using gentle, circular motions to avoid irritating the gums. Floss daily to remove debris between teeth, and consider incorporating an antimicrobial mouthwash to reduce bacterial growth. For those at higher risk, such as smokers or individuals with a genetic predisposition, regular dental check-ups every three to four months are essential. Additionally, addressing habits like teeth grinding or aggressive brushing can significantly reduce the risk of recession.
Comparatively, while mild gum recession may only cause minor discomfort, advanced cases can lead to severe complications. For instance, exposed roots are more susceptible to cavities, as they lack the protective enamel found on the tooth crown. In extreme cases, the supporting bone structure may deteriorate, leading to tooth mobility. Unlike early-stage gum disease, which may be reversible with proper care, advanced recession often requires surgical intervention, such as gum grafting, to restore lost tissue and protect the teeth.
In conclusion, receding gums are a visible and serious symptom of advanced gum disease that demand attention. By recognizing the signs early, maintaining rigorous oral care, and seeking professional treatment, you can mitigate the risks and preserve your dental health. Remember, the roots of your teeth are not meant to be exposed—protecting your gums is essential for a healthy, lasting smile.
Cost of Gum Disease Treatment: What to Expect and Budget For
You may want to see also

Persistent bad breath: Halitosis can result from bacteria buildup and infection in the gums and teeth
Bad breath, or halitosis, is more than just an embarrassing social inconvenience—it can be a red flag for underlying gum disease. When bacteria accumulate in the mouth, they produce volatile sulfur compounds (VSCs), which are the primary culprits behind that persistent, unpleasant odor. This bacterial buildup often thrives in environments where gum health is compromised, such as in cases of gingivitis or periodontitis. If you notice your breath remains foul despite regular brushing and mouthwash use, it’s time to investigate further, as this could indicate an infection in the gums or teeth.
To address halitosis linked to gum disease, start with a thorough oral hygiene routine. Brush twice daily with a fluoride toothpaste, ensuring you clean the gum line where bacteria tend to hide. Flossing is non-negotiable—it removes debris and plaque between teeth that brushing alone can’t reach. For an extra antimicrobial boost, consider using an alcohol-free mouthwash containing chlorhexidine (0.12% concentration) twice daily, but consult your dentist first, as long-term use can stain teeth. Additionally, cleaning your tongue with a scraper or brush can eliminate bacteria residing on its surface, significantly reducing VSC production.
Diet and hydration play a critical role in managing halitosis. Dehydration reduces saliva flow, which allows bacteria to flourish, so aim for at least 8 glasses of water daily. Avoid foods high in sugar or acid, as they create an ideal environment for bacterial growth. Instead, incorporate crunchy fruits and vegetables like apples or carrots, which act as natural toothbrushes, stimulating saliva production and scrubbing away plaque. Chewing sugar-free gum with xylitol can also help, as it neutralizes acids and promotes saliva flow.
If these measures don’t resolve your bad breath, it’s essential to seek professional care. Persistent halitosis may signal advanced gum disease, tooth decay, or even systemic issues like diabetes. A dentist can perform a comprehensive exam, including periodontal probing to assess gum health and X-rays to detect hidden infections. Treatment might involve deep cleaning (scaling and root planing) to remove plaque and tartar below the gum line, or antibiotics if the infection is severe. Early intervention not only freshens your breath but also prevents irreversible damage to your gums and teeth.
In summary, persistent bad breath is more than a nuisance—it’s a symptom demanding attention. By maintaining rigorous oral hygiene, making smart dietary choices, and seeking timely dental care, you can eliminate halitosis and safeguard your gum health. Remember, fresh breath isn’t just about confidence; it’s a reflection of your overall oral well-being.
Effective Home Remedies to Treat Gum Disease Without Dental Visits
You may want to see also

Loose or shifting teeth: Advanced gum disease damages bone support, causing teeth to feel loose or move
One of the most alarming signs of advanced gum disease is the sensation of loose or shifting teeth. This occurs because the disease, known as periodontitis, progressively destroys the bone and tissue that anchor your teeth in place. As the supportive structures weaken, teeth lose their stability, leading to noticeable movement or wobbling. This is not a natural part of aging but a clear warning sign that immediate dental intervention is needed.
Imagine biting into an apple and feeling your tooth shift uncomfortably, or noticing a gap widening between teeth that once fit snugly together. These are not minor inconveniences but indicators of severe bone loss. At this stage, the damage is often irreversible, making early detection and treatment critical. Regular dental check-ups, especially for adults over 40, can help identify gum disease before it reaches this advanced state.
To prevent progression, dentists may recommend deep cleaning procedures like scaling and root planing to remove plaque and tartar below the gumline. In severe cases, surgical interventions such as bone grafts or flap surgery may be necessary to restore support. At home, maintaining impeccable oral hygiene—brushing twice daily, flossing, and using antimicrobial mouthwash—can slow the disease’s advancement. However, once teeth begin to loosen, professional care is non-negotiable.
Comparing this to other symptoms of gum disease, such as bleeding gums or bad breath, loose teeth are a late-stage red flag. While bleeding gums might be ignored as minor, loose teeth demand urgent attention. They signify that the disease has progressed beyond the gums and is now compromising the jawbone. Ignoring this symptom can lead to tooth loss, which not only affects appearance but also impacts chewing ability and overall oral health.
In conclusion, loose or shifting teeth are a stark reminder of the destructive power of advanced gum disease. They are not a condition to be managed at home but a call to action for professional dental care. By recognizing this symptom early and seeking treatment, you can preserve your natural teeth and prevent further damage to your oral health.
Recognizing Early Signs of Periodontal Disease: Symptoms and Prevention Tips
You may want to see also
Frequently asked questions
Early signs include red, swollen, or tender gums, bleeding while brushing or flossing, and persistent bad breath.
Yes, gum disease can cause gums to recede, appear bright red or purple, and pull away from the teeth, creating pockets.
Advanced gum disease (periodontitis) may show symptoms like loose teeth, pus between gums and teeth, and significant gum recession.
Yes, gum disease can make teeth appear longer due to receding gums and may cause teeth to shift or become misaligned.
Yes, early-stage gum disease (gingivitis) often presents as slight gum inflammation, bleeding gums, and mild redness around the gum line.















