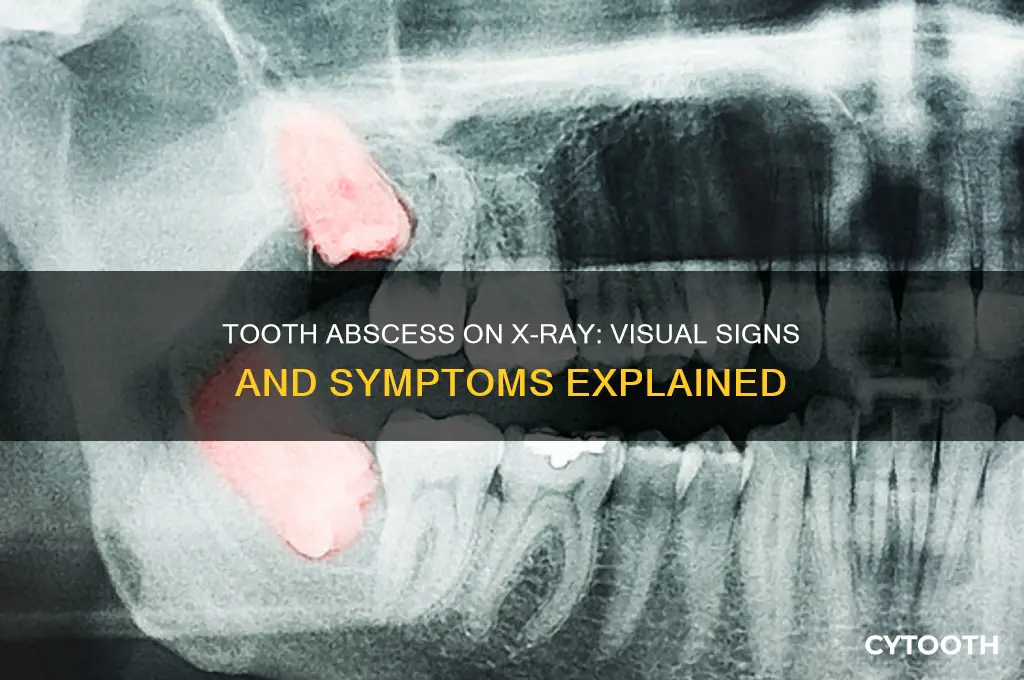
A tooth abscess, a painful infection at the root of a tooth or between the gum and a tooth, can often be identified on an X-ray as a dark spot or area of radiolucency, indicating the presence of pus or inflammation. This radiographic image typically reveals a well-defined, round or oval-shaped lesion surrounding the affected tooth, which may appear as a shadow or a darker region compared to the surrounding bone. Dentists rely on X-rays as a crucial diagnostic tool to detect abscesses, as they provide a clear visualization of the infection's extent and its impact on the tooth and surrounding structures, aiding in prompt treatment and preventing further complications.
| Characteristics | Values |
|---|---|
| Location | Typically appears at the apex (tip) of the tooth root, but can also be seen laterally or periapically (around the root). |
| Appearance | Radiolucent (dark) area indicating bone destruction or resorption. |
| Shape | Often round or oval, but can be irregular depending on the extent of the infection. |
| Margins | May have well-defined or poorly defined borders, depending on the stage of the abscess. |
| Size | Varies from small to large, depending on the severity and duration of the infection. |
| Associated Findings | Periapical rarefaction (loss of bone density), widening of the periodontal ligament space, or cortical bone erosion in advanced cases. |
| Tooth Involvement | The affected tooth may show signs of decay, a large restoration, or a non-vital (dead) pulp. |
| Differential Diagnosis | Must be distinguished from other radiolucent lesions like cysts, granulomas, or tumors based on clinical and radiographic features. |
| Limitations | Early-stage abscesses may not be visible on X-rays; advanced imaging like CBCT may be needed for confirmation. |
What You'll Learn
- Abscess Location: Identifying where the abscess appears in relation to the tooth and surrounding structures
- Bone Destruction: Detecting areas of bone loss caused by the infection on the x-ray
- Periapical Abscess: Appearance of a dark, radiolucent area at the tooth's root tip
- Periodontal Abscess: X-ray shows localized bone loss near the gum line, indicating infection
- Radiographic Signs: Key indicators like widening of the periodontal ligament space or fuzzy bone edges

Abscess Location: Identifying where the abscess appears in relation to the tooth and surrounding structures
On a dental X-ray, the location of a tooth abscess is a critical diagnostic clue. Abscesses typically manifest as radiolucent areas, appearing darker than the surrounding bone due to the destruction of mineralized tissue. These lesions can be situated in various locations relative to the tooth, each indicating a different origin and progression of the infection. For instance, a periapical abscess, the most common type, appears at the apex of the tooth root, often as a well-defined dark area surrounded by a sclerotic (dense) border, reflecting the body’s attempt to contain the infection.
To identify the abscess location, start by examining the tooth’s root structure. A periapical abscess will be directly adjacent to the root tip, while a periodontal abscess appears between the root and the alveolar bone, often with a loss of the periodontal ligament space. In contrast, a pericoronal abscess, typically seen with impacted teeth, forms above the crown, visible as a radiolucent area surrounding the unerupted tooth. Understanding these patterns is essential for accurate diagnosis and treatment planning, as the location dictates the approach—whether it’s root canal therapy, incision and drainage, or surgical intervention.
When analyzing the X-ray, consider the relationship between the abscess and surrounding structures. For example, an abscess near the maxillary sinus may indicate sinus involvement, requiring careful management to prevent complications. Similarly, an abscess extending into the mandibular canal could compress the inferior alveolar nerve, causing numbness or pain. These anatomical considerations highlight the importance of precise localization, as misidentification can lead to inadequate treatment or further damage.
Practical tips for radiographic interpretation include using cone-beam computed tomography (CBCT) for complex cases, as it provides 3D imaging to better assess the extent and location of the abscess. Additionally, compare current and previous X-rays to track progression or resolution, especially in chronic cases. For dental professionals, mastering abscess localization on X-rays is not just about diagnosis—it’s about tailoring treatment to the patient’s unique anatomy and condition, ensuring effective and minimally invasive care.
Identifying a Dog Tooth Abscess: Symptoms and Visual Signs
You may want to see also

Bone Destruction: Detecting areas of bone loss caused by the infection on the x-ray
Bone destruction is a telltale sign of a tooth abscess on an x-ray, manifesting as radiolucent areas where the infection has eroded the alveolar bone. These dark zones contrast sharply with the denser, lighter appearance of healthy bone, making them relatively easy to identify. The extent of bone loss can vary, ranging from small, localized defects to extensive destruction that compromises the integrity of the tooth's supporting structures. Radiologists and dentists often look for these characteristic changes to confirm the presence and severity of an abscess.
To detect bone destruction accurately, it’s crucial to examine the periapical region—the area surrounding the tooth's root tip. This is where abscesses commonly cause bone resorption, leading to a loss of the normal, sharp margin of the alveolar crest. In advanced cases, the lamina dura, a thin, dense line of bone adjacent to the tooth root, may appear discontinuous or completely absent. Comparing the affected area to the contralateral side or adjacent teeth can provide a baseline for assessing the extent of damage. Digital radiography, with its enhanced contrast and magnification capabilities, is particularly useful for pinpointing subtle changes in bone density.
While bone destruction is a key indicator, it’s important to interpret x-ray findings in context. Not all abscesses cause immediate or visible bone loss, especially in the early stages. For instance, a localized periodontal abscess may show minimal bone changes initially, while a chronic periapical abscess often presents with more pronounced destruction. Clinicians should correlate radiographic evidence with clinical symptoms, such as swelling, pain, or drainage, to make an accurate diagnosis. In cases where bone loss is extensive, additional imaging modalities like cone-beam computed tomography (CBCT) may be necessary to evaluate the three-dimensional extent of the damage.
Practical tips for identifying bone destruction include adjusting the x-ray’s contrast and brightness to highlight subtle radiolucent areas. Dentists should also pay attention to the pattern of bone loss—whether it’s circumscribed or diffuse—as this can provide clues about the nature and duration of the infection. For example, a well-defined radiolucency often suggests a chronic abscess, while a more diffuse pattern may indicate acute, rapidly progressing infection. Early detection is critical, as significant bone loss can lead to tooth mobility, tooth loss, or even spread of the infection to adjacent structures.
In conclusion, recognizing bone destruction on an x-ray is a vital skill for diagnosing tooth abscesses. By focusing on radiolucent areas, changes in the lamina dura, and the periapical region, clinicians can accurately assess the extent of infection-related bone loss. Combining radiographic findings with clinical symptoms ensures a comprehensive diagnosis, enabling timely intervention to prevent further complications. Mastery of this technique not only aids in patient care but also underscores the importance of radiography in modern dental practice.
Ruptured Tooth Abscess: Visual Symptoms, Risks, and Immediate Care Guide
You may want to see also

Periapical Abscess: Appearance of a dark, radiolucent area at the tooth's root tip
A periapical abscess manifests on an x-ray as a distinct dark area at the apex of the tooth’s root, a radiolucent zone that contrasts sharply with the surrounding bone. This darkness results from the breakdown of bone tissue caused by bacterial infection, which replaces dense bone with fluid-filled space. Radiologists and dentists identify this feature as a hallmark of periapical abscesses, differentiating it from other dental pathologies like periodontal disease or cysts. The clarity of this radiolucent area is critical for diagnosis, as it directly correlates with the extent of infection and guides treatment decisions.
Analyzing the x-ray image, the size and shape of the radiolucent area provide insights into the abscess’s progression. A small, well-defined lesion may indicate an early-stage infection, while a larger, irregular area suggests advanced bone destruction. For instance, a periapical abscess in its initial phase might appear as a subtle, round radiolucency measuring 2–3 mm, whereas chronic cases can exhibit lesions exceeding 10 mm with jagged borders. Dentists often compare current x-rays with previous ones to track changes, ensuring timely intervention before irreversible damage occurs.
To interpret these findings effectively, clinicians must consider patient symptoms alongside radiographic evidence. Pain, swelling, and sensitivity to pressure are common indicators of an active abscess, but asymptomatic cases are not uncommon, particularly in chronic infections. In such scenarios, the x-ray becomes the primary diagnostic tool. For example, a patient with no reported pain but a 5 mm radiolucent area on an x-ray may still require root canal therapy to prevent further bone loss. This underscores the importance of routine dental x-rays, especially for high-risk groups like adults over 40 or individuals with poor oral hygiene.
Practical tips for patients include monitoring for subtle signs of infection, such as a persistent bad taste or slight gum discomfort, which may precede visible swelling. If a periapical abscess is suspected, avoiding hot or cold foods can minimize pain temporarily, but professional treatment is non-negotiable. Dentists typically prescribe antibiotics to control the infection, followed by root canal treatment or extraction to eliminate the source. Post-treatment care, including warm salt-water rinses and adherence to prescribed medications, is crucial to prevent recurrence. Early detection through regular x-rays remains the most effective strategy to manage periapical abscesses and preserve dental health.
Identifying Cat Tooth Abscesses: Symptoms, Appearance, and Treatment Options
You may want to see also

Periodontal Abscess: X-ray shows localized bone loss near the gum line, indicating infection
A periodontal abscess is a localized infection that occurs in the gum tissue, often as a result of advanced gum disease or a deep periodontal pocket. When examining an X-ray of a periodontal abscess, one of the most telling signs is localized bone loss near the gum line. This bone loss, also known as alveolar bone resorption, appears as a dark, radiolucent area adjacent to the affected tooth. The contrast between the healthy, dense bone and the eroded area is stark, making it a critical diagnostic feature. This X-ray finding not only confirms the presence of infection but also highlights the extent of tissue damage caused by the abscess.
Analyzing the X-ray further, the bone loss typically follows the contour of the periodontal pocket, indicating that the infection has spread from the soft tissues into the supporting bone structures. This pattern distinguishes a periodontal abscess from other types of dental infections, such as periapical abscesses, which show bone loss at the root apex. The localized nature of the bone destruction in periodontal abscesses underscores the importance of early intervention to prevent further progression of gum disease. Dentists often use this X-ray evidence to tailor treatment plans, which may include deep cleaning (scaling and root planing), antibiotic therapy, or surgical intervention to remove infected tissue.
From a practical standpoint, patients with a periodontal abscess may not always exhibit obvious symptoms like swelling or pain, making X-rays an indispensable tool for diagnosis. For individuals over the age of 30, routine dental X-rays every 1–2 years are recommended, especially if there is a history of gum disease or poor oral hygiene. If localized bone loss is detected, it’s crucial to address the underlying infection promptly. Delaying treatment can lead to irreversible bone damage, tooth mobility, and even tooth loss. Maintaining good oral hygiene practices, including twice-daily brushing, daily flossing, and regular dental check-ups, can significantly reduce the risk of developing a periodontal abscess.
Comparatively, while periapical abscesses often present with a well-defined radiolucent area at the root tip, periodontal abscesses show bone loss confined to the gum line. This distinction is vital for accurate diagnosis and treatment planning. For instance, a periapical abscess may require root canal therapy, whereas a periodontal abscess focuses on managing gum disease. Understanding these differences ensures that patients receive the most effective care. Additionally, X-rays allow dentists to monitor the progression of bone loss over time, providing valuable insights into the effectiveness of treatment and the need for adjustments in the patient’s oral care regimen.
In conclusion, an X-ray of a periodontal abscess revealing localized bone loss near the gum line is a clear indicator of infection and advanced gum disease. This finding not only aids in diagnosis but also guides treatment strategies to halt disease progression and preserve oral health. By recognizing this specific X-ray pattern, both dentists and patients can take proactive steps to address the infection and prevent long-term complications. Regular dental imaging and adherence to recommended oral hygiene practices are essential in managing and preventing periodontal abscesses.
Identifying Tooth Abscess Symptoms: Visual Signs and What to Look For
You may want to see also

Radiographic Signs: Key indicators like widening of the periodontal ligament space or fuzzy bone edges
A tooth abscess on an x-ray often reveals subtle yet distinct radiographic signs that signal underlying infection. One of the most telling indicators is the widening of the periodontal ligament (PDL) space. Normally, the PDL space appears as a thin, uniform radiolucent line surrounding the tooth root. However, in the presence of an abscess, this space becomes abnormally widened due to inflammation and fluid accumulation. This change is particularly noticeable in periapical abscesses, where the infection originates at the root tip. Dentists often compare the affected PDL space to the contralateral tooth or adjacent teeth for a more accurate diagnosis.
Another critical radiographic sign is fuzzy or ill-defined bone edges adjacent to the infected tooth. Healthy bone appears sharp and well-defined on x-rays, but an abscess can cause bone resorption, leading to a blurred or hazy appearance. This occurs as the body’s immune response to the infection begins to break down bone tissue. The extent of fuzziness can indicate the severity of the abscess, with more pronounced changes suggesting advanced infection. Radiologists and dentists use this feature to assess the progression of the condition and plan appropriate treatment.
While these signs are highly indicative, their interpretation requires careful consideration of other factors. For instance, patient age and medical history can influence radiographic appearance. Younger patients may show more rapid bone changes due to higher metabolic activity, while older adults might exhibit slower progression. Additionally, radiographic technique plays a crucial role; overexposure or underexposure can distort the PDL space or bone edges, leading to misdiagnosis. Standardizing x-ray settings and using digital radiography can enhance accuracy.
To maximize diagnostic utility, clinicians should follow a systematic approach. Step 1: Compare the affected area to the contralateral side to identify asymmetry in the PDL space or bone structure. Step 2: Assess the periapical region for radiolucency, which often accompanies abscesses. Step 3: Evaluate the surrounding bone for cortical plate disruption or loss. Caution: Relying solely on x-rays can be misleading, as early-stage abscesses may not show radiographic changes. Clinical symptoms like pain, swelling, and tenderness should always be considered alongside imaging.
In conclusion, recognizing radiographic signs such as widened PDL space and fuzzy bone edges is essential for diagnosing tooth abscesses. These indicators, when interpreted in conjunction with clinical findings and patient history, provide a comprehensive understanding of the infection’s extent. By mastering these nuances, dental professionals can ensure timely and effective treatment, preventing complications like systemic infection or bone loss.
Effective Treatments for Tooth Abscess: What Dentists Do to Relieve Pain
You may want to see also
Frequently asked questions
On an x-ray, a tooth abscess typically appears as a dark or radiolucent area near the root of the affected tooth, indicating bone loss or a pocket of infection.
Not always. Early-stage abscesses may not be visible on x-rays, but as the infection progresses, bone destruction or a radiolucent lesion becomes more apparent.
Additional signs include widening of the periodontal ligament space, periapical radiolucency (darkening around the tooth's root), or loss of lamina dura (a thin layer of bone surrounding the tooth).
An x-ray provides a detailed view of the tooth's internal structures and surrounding bone, revealing hidden infections or damage that may not be visible during a visual exam.















