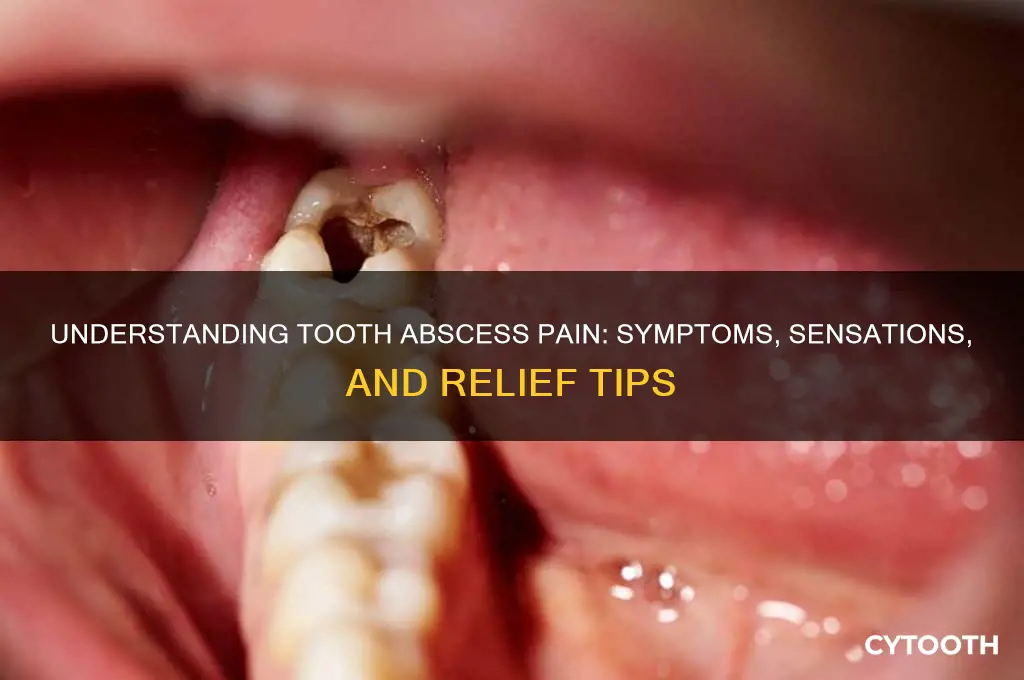
A tooth abscess is a painful infection that occurs when bacteria invade the dental pulp or the tissues surrounding a tooth, often due to decay, gum disease, or injury. The pain associated with a tooth abscess can be intense and throbbing, typically worsening when lying down or applying pressure to the affected area. It may radiate to the jaw, ear, or neck, making it difficult to pinpoint the exact source. Other common symptoms include swelling in the face or cheek, sensitivity to hot or cold, a persistent bad taste or odor in the mouth, and sometimes fever or general malaise. If left untreated, the infection can spread, leading to more serious health complications, making prompt dental care essential.
| Characteristics | Values |
|---|---|
| Pain | Severe, throbbing, or sharp pain in or around the affected tooth. |
| Swelling | Swelling in the face, cheek, or jaw near the infected tooth. |
| Sensitivity | Increased sensitivity to hot, cold, or pressure on the tooth. |
| Redness | Redness or inflammation in the gums around the abscessed tooth. |
| Bad Taste or Smell | Foul taste in the mouth or bad breath due to pus or infection. |
| Fever | Possible low-grade fever as a systemic response to infection. |
| Difficulty Chewing | Pain or discomfort when chewing or biting with the affected tooth. |
| Swollen Lymph Nodes | Tender or swollen lymph nodes in the neck or under the jaw. |
| Pus Drainage | Visible pus or fluid draining from the gum near the infected tooth. |
| Tooth Mobility | The affected tooth may feel loose due to the infection spreading. |
| General Malaise | Feeling unwell, fatigued, or generally ill due to the infection. |
| Pain Radiation | Pain may radiate to the ear, jaw, or neck on the same side as the abscess. |
| Gum Bump | A visible bump (parulis) on the gum near the infected tooth. |
| Difficulty Opening Mouth | Swelling or pain may make it difficult to open the mouth fully. |
What You'll Learn
- Throbbing Pain: Persistent, intense pain in the affected tooth, often worsening when lying down
- Swelling: Noticeable swelling in the face, cheek, or jaw near the abscess
- Sensitivity: Extreme sensitivity to hot, cold, or pressure on the infected tooth
- Fever: Low-grade fever, chills, and general malaise due to infection spreading
- Bad Taste/Smell: Foul taste or odor in the mouth from pus drainage

Throbbing Pain: Persistent, intense pain in the affected tooth, often worsening when lying down
A tooth abscess doesn’t whisper its presence—it roars. Among its most defining symptoms is a throbbing pain that feels like a relentless pulse in the affected tooth. This isn’t the fleeting discomfort of a minor cavity; it’s a persistent, intense ache that demands attention. The pain often radiates to the jaw, ear, or neck, creating a symphony of misery. What’s worse? It intensifies when lying down. Gravity shifts blood flow to the head, increasing pressure in the abscessed area, turning a bad situation into a sleepless nightmare.
To manage this pain temporarily, over-the-counter analgesics like ibuprofen (600–800 mg every 6–8 hours) or acetaminophen (500–1000 mg every 4–6 hours) can provide relief. However, these are stopgap measures, not solutions. Applying a cold compress to the cheek for 15–20 minutes can also reduce inflammation and numb the area. Avoid heat, as it may worsen swelling. For immediate comfort, prop yourself up with extra pillows when resting—keeping your head elevated minimizes blood flow to the abscess, temporarily easing the throbbing.
Comparing this pain to other dental issues highlights its severity. A cavity might cause sensitivity to hot or cold, but an abscessed tooth feels like a constant, deep-seated battle. Unlike gum inflammation, which may subside with proper care, abscess pain persists and escalates. It’s a clear signal of infection, often stemming from untreated decay or a cracked tooth, that requires urgent dental intervention. Ignoring it risks the infection spreading to the jawbone, bloodstream, or even the brain—a potentially life-threatening scenario.
The throbbing nature of the pain is your body’s alarm system, signaling that the infection is active and aggressive. It’s not just discomfort; it’s a symptom of pus buildup at the tooth’s root. This pressure exacerbates the pain, especially in a reclined position. If you’re experiencing this, avoid chewing on the affected side and rinse your mouth gently with warm saltwater to reduce bacterial activity. But remember: home remedies are temporary fixes. A dentist will likely drain the abscess, prescribe antibiotics (such as amoxicillin 500 mg, 3 times daily for 7–10 days), and address the root cause, whether through a root canal or extraction.
In essence, throbbing pain from a tooth abscess is more than a nuisance—it’s a red flag. Its persistence, intensity, and positional worsening are telltale signs of a deep infection. While quick fixes like painkillers and cold packs can offer fleeting relief, professional treatment is non-negotiable. Delaying care risks complications far beyond a painful tooth. Listen to your body’s cry for help and act swiftly.
Abscessed Tooth Treatment: What to Expect and How to Heal
You may want to see also

Swelling: Noticeable swelling in the face, cheek, or jaw near the abscess
One of the most visible and alarming symptoms of a tooth abscess is the swelling that occurs in the face, cheek, or jaw near the affected area. This swelling is your body’s inflammatory response to the infection, as white blood cells rush to fight the bacteria. It typically appears as a firm, tender bulge that may feel warm to the touch. Unlike minor puffiness from a cold or allergy, abscess-related swelling is localized, persistent, and often worsens over time. If left untreated, it can spread to adjacent tissues, causing further discomfort and potential complications.
To manage this swelling, apply a cold compress to the affected area for 15–20 minutes at a time, repeating every few hours. This can help reduce inflammation and numb the pain temporarily. Over-the-counter anti-inflammatory medications like ibuprofen (200–400 mg every 4–6 hours, as directed by a pharmacist or doctor) may also provide relief. However, these measures are palliative and do not address the underlying infection. Avoid applying heat, as it can increase blood flow and worsen the swelling.
Comparing abscess swelling to other facial conditions can help differentiate it. Unlike the generalized swelling of sinusitis or allergies, abscess-related swelling is usually confined to one side of the face and directly linked to a specific tooth. It also differs from the soft, movable fluid retention seen in conditions like angioedema, as abscess swelling is firmer and tied to an infection source. If you notice swelling accompanied by severe pain, fever, or difficulty swallowing, seek immediate dental or medical attention, as these could indicate a spreading infection.
For children or older adults, swelling from a tooth abscess can be particularly concerning due to their potentially weaker immune responses. Parents should monitor for signs of swelling in children, who may not articulate pain clearly. In older adults, especially those with diabetes or compromised immune systems, swelling can progress rapidly, increasing the risk of systemic infection. In all cases, early intervention is critical. A dentist can drain the abscess, prescribe antibiotics (such as amoxicillin 500 mg three times daily for adults, adjusted for age and weight in children), and recommend follow-up care to prevent recurrence.
Tooth Abscess Burst: Immediate Steps and Emergency Care Guide
You may want to see also

Sensitivity: Extreme sensitivity to hot, cold, or pressure on the infected tooth
A tooth abscess doesn’t whisper its presence—it screams. Among its most unmistakable symptoms is extreme sensitivity to temperature and pressure. Imagine sipping a warm coffee or biting into an apple, only to be met with a jolt of pain so sharp it feels like your tooth is wired to an electric current. This isn’t mere discomfort; it’s a distress signal from your body, alerting you to an infection that demands immediate attention.
The science behind this sensitivity lies in the inflammation of the tooth’s pulp, where nerves are exposed due to decay or trauma. When hot or cold substances touch the affected area, these nerves react violently, amplifying the sensation. Pressure, whether from chewing or even brushing, triggers a similar response. For adults, this can be particularly debilitating, as the pain often radiates to the jaw or ear, making it difficult to pinpoint the source without professional diagnosis.
Children and older adults may exhibit unique responses to this sensitivity. Kids, for instance, might refuse to eat or drink anything but lukewarm foods, while seniors with diminished nerve sensitivity may still experience pain but describe it as a persistent, dull ache rather than a sharp sting. Regardless of age, the takeaway is clear: this sensitivity is not a minor inconvenience—it’s a red flag signaling an abscess that, if left untreated, can lead to systemic infection or tooth loss.
Practical tips for managing this symptom temporarily include avoiding extreme temperatures and opting for soft, room-temperature foods. Over-the-counter pain relievers like ibuprofen (200–400 mg every 4–6 hours for adults) can provide short-term relief, but they are not a substitute for treatment. Rinsing with warm saltwater may soothe the area, but it’s a bandage on a bullet wound. The only effective solution is to see a dentist promptly, who may prescribe antibiotics or perform a root canal to eliminate the infection and restore comfort.
In comparison to other dental issues, this sensitivity is far more intense and persistent. A cavity might cause mild discomfort, but an abscessed tooth’s reaction to stimuli is immediate and severe. It’s the difference between a flicker of annoyance and a full-blown alarm. Ignoring it is not an option—the pain will only worsen, and the infection can spread, turning a localized problem into a systemic crisis. Act fast, because when it comes to a tooth abscess, sensitivity isn’t just a symptom—it’s a warning you can’t afford to ignore.
Effective Treatments for Tooth Abscess: What Dentists Do to Relieve Pain
You may want to see also

Fever: Low-grade fever, chills, and general malaise due to infection spreading
A tooth abscess is more than just a localized dental issue; it can trigger systemic responses as the infection spreads. One of the most telling signs of this progression is the onset of a low-grade fever, often accompanied by chills and a pervasive sense of malaise. These symptoms signal that the body is mounting a defense against the infection, but they also indicate that the abscess has advanced beyond a simple toothache. Ignoring these signs can lead to more severe complications, making it crucial to recognize and address them promptly.
Analyzing the fever associated with a tooth abscess reveals its role as a red flag. A low-grade fever, typically ranging between 100°F and 101°F (37.8°C to 38.3°C), is the body’s attempt to kill off invading bacteria. Chills often accompany this fever as the body’s temperature regulation system fluctuates. General malaise, characterized by fatigue, weakness, and a lack of energy, further underscores the systemic impact of the infection. These symptoms collectively highlight that the abscess is no longer confined to the tooth but is affecting the body as a whole.
For those experiencing these symptoms, immediate action is essential. Over-the-counter fever reducers like acetaminophen (500–1000 mg every 4–6 hours for adults) can provide temporary relief, but they do not address the root cause. Hydration is critical to support the immune system, with adults aiming for at least 8–10 glasses of water daily. However, self-treatment should never replace professional care. A dentist or healthcare provider must be consulted to drain the abscess and prescribe antibiotics, such as amoxicillin (500 mg every 8 hours for adults), to combat the infection effectively.
Comparing these symptoms to those of a common cold or flu can be misleading. While both conditions may present with fever and malaise, the localized dental pain and swelling associated with a tooth abscess are key differentiators. Unlike viral illnesses, which often resolve within a week, an untreated tooth abscess will worsen, potentially leading to sepsis or other life-threatening conditions. This distinction underscores the urgency of seeking dental care rather than waiting for symptoms to subside on their own.
In conclusion, a low-grade fever, chills, and general malaise are not mere inconveniences but critical indicators of a spreading tooth abscess. Recognizing these symptoms early, understanding their significance, and taking immediate steps to address the infection can prevent severe health complications. While temporary relief measures can help manage discomfort, professional intervention is non-negotiable. Treating a tooth abscess as a dental emergency ensures not only the preservation of oral health but also the protection of overall well-being.
Tooth Abscess Treatment: Immediate Steps and When to See a Dentist
You may want to see also

Bad Taste/Smell: Foul taste or odor in the mouth from pus drainage
A tooth abscess is more than just a localized infection; it’s a full-body alarm system signaling something is critically wrong. Among its most unsettling symptoms is the foul taste or odor in the mouth caused by pus drainage. This isn’t merely unpleasant—it’s a red flag. The taste often resembles a metallic or salty bitterness, lingering even after brushing or rinsing. The odor, similarly, is sharp and offensive, detectable not just by the individual but often by those nearby. These symptoms arise from the body’s attempt to expel infected material, a process that, while protective, can be deeply distressing.
To manage this symptom temporarily, rinse your mouth with a warm saltwater solution (1/2 teaspoon of salt in 8 ounces of water) every 2–3 hours. Avoid alcohol-based mouthwashes, as they can irritate the abscess. Chewing sugar-free gum or sucking on sugar-free lozenges may stimulate saliva production, helping to dilute the foul taste. However, these measures are palliative, not curative. The underlying infection must be addressed by a dentist, who may prescribe antibiotics (e.g., amoxicillin 500 mg every 8 hours for adults) or perform a drainage procedure.
Comparatively, the bad taste and smell from a tooth abscess differ from those caused by poor oral hygiene or dietary factors. While brushing after a garlicky meal might leave a temporary odor, the abscess-related symptoms persist and worsen over time. They’re often accompanied by other signs like throbbing pain, swelling, and fever, forming a distinct cluster of symptoms that demand immediate attention. Ignoring these signs can lead to systemic complications, such as sepsis, making prompt treatment non-negotiable.
Descriptively, the experience is akin to having a spoonful of spoiled food trapped in your mouth, impossible to spit out or wash away. The odor can be so potent that it affects your appetite, making eating or drinking a chore. For children or elderly individuals, this can lead to dehydration or malnutrition if not managed promptly. Caregivers should monitor fluid intake and encourage soft, cool foods like yogurt or smoothies, which are less likely to aggravate the sensitive area.
Persuasively, the bad taste and smell from a tooth abscess are not just nuisances—they’re cries for help from your body. Delaying treatment risks the infection spreading to the jawbone, bloodstream, or brain. If you notice these symptoms, especially alongside facial swelling or difficulty swallowing, seek emergency dental care. Early intervention not only alleviates discomfort but also prevents long-term damage, saving both your tooth and your overall health.
Tooth Abscess Popped? Immediate Steps to Take for Relief and Recovery
You may want to see also
Frequently asked questions
Common symptoms include severe, throbbing toothache, sensitivity to hot or cold, fever, swollen face or cheek, tender lymph nodes, bad breath, and a foul taste in the mouth.
The pain from a tooth abscess can be constant and intense, but it may also come and go initially. As the infection worsens, the pain typically becomes more persistent.
Yes, a tooth abscess can cause noticeable swelling in the face, jaw, or gums near the infected tooth. This swelling may be accompanied by redness and warmth in the affected area.
The pain from a tooth abscess is often described as severe, throbbing, and radiating to the jaw, ear, or neck. It is usually more intense and persistent than a typical toothache.