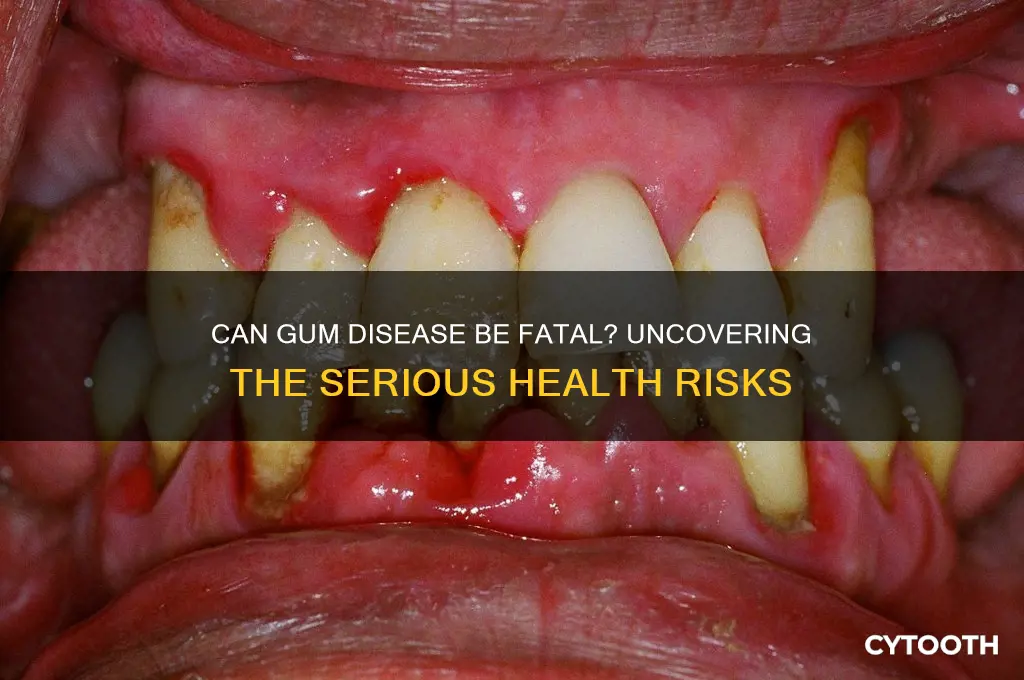
Gum disease, also known as periodontal disease, is a common oral health issue caused by bacterial infection and inflammation of the gums. While it typically starts as gingivitis, a mild form characterized by redness and swelling, it can progress to periodontitis, which affects the bone supporting the teeth. Although gum disease is not directly fatal, its advanced stages can lead to severe complications, including tooth loss, systemic inflammation, and an increased risk of cardiovascular disease, diabetes, and respiratory infections. Addressing gum disease early through proper oral hygiene, regular dental check-ups, and timely treatment is crucial to prevent these potentially life-threatening complications.
| Characteristics | Values |
|---|---|
| Direct Cause of Death | Gum disease itself is not a direct cause of death. |
| Indirect Health Risks | Linked to serious systemic conditions like heart disease, diabetes, and stroke. |
| Severity of Gum Disease | Advanced stages (periodontitis) pose higher risks than gingivitis. |
| Systemic Inflammation | Chronic inflammation from gum disease can exacerbate other health issues. |
| Cardiovascular Risk | Increased risk of heart attack, stroke, and atherosclerosis. |
| Diabetes Complications | Worsens blood sugar control, increasing diabetes-related complications. |
| Respiratory Infections | Linked to pneumonia and chronic obstructive pulmonary disease (COPD). |
| Pregnancy Complications | Associated with preterm birth and low birth weight. |
| Alzheimer's Disease | Recent studies suggest a potential link to cognitive decline. |
| Cancer Risk | Some studies indicate a higher risk of certain cancers (e.g., pancreatic). |
| Mortality Rate Impact | Indirectly contributes to higher mortality rates via associated conditions. |
| Preventability | Highly preventable with proper oral hygiene and regular dental care. |
| Treatment Effectiveness | Early treatment reduces risks, but advanced cases may have lasting effects. |
| Global Prevalence | Affects over 50% of adults worldwide, increasing potential health impacts. |
| Economic Burden | Significant healthcare costs due to associated systemic conditions. |
| Public Awareness | Low awareness of the link between gum disease and systemic health risks. |
What You'll Learn
- Gum Disease and Heart Health: Links between gum disease and cardiovascular issues, including potential risks
- Systemic Infections: How gum disease can lead to severe systemic infections if left untreated
- Diabetes Complications: Impact of gum disease on diabetes management and overall health risks
- Respiratory Problems: Connection between gum disease and respiratory conditions like pneumonia
- Cancer Risks: Studies suggesting a potential link between gum disease and certain cancers

Gum Disease and Heart Health: Links between gum disease and cardiovascular issues, including potential risks
Gum disease, or periodontal disease, isn't just a threat to your oral health—it may also jeopardize your cardiovascular system. Research increasingly highlights a connection between gum inflammation and heart conditions, suggesting that the bacteria and inflammation in your mouth can travel through the bloodstream, affecting your heart. For instance, studies show that individuals with gum disease are nearly twice as likely to develop heart disease compared to those with healthy gums. This link underscores the importance of oral hygiene not just for a bright smile, but for a healthy heart.
Consider the mechanism behind this connection: harmful oral bacteria can enter the bloodstream through inflamed gums, leading to systemic inflammation and arterial damage. Over time, this can contribute to atherosclerosis, a condition where arteries narrow due to plaque buildup, increasing the risk of heart attacks and strokes. For example, *Porphyromonas gingivalis*, a bacterium associated with gum disease, has been found in arterial plaques of heart disease patients. This isn’t mere coincidence—it’s a biological pathway that ties oral neglect to cardiovascular risks.
Practical steps to mitigate these risks include maintaining rigorous oral hygiene: brush twice daily with fluoride toothpaste, floss daily, and use an antimicrobial mouthwash. Adults over 30, in particular, should schedule dental check-ups every six months, as gum disease becomes more prevalent with age. Additionally, quitting smoking is critical, as tobacco use exacerbates both gum disease and cardiovascular issues. Diet also plays a role—limit sugary foods and beverages, which fuel harmful oral bacteria, and incorporate heart-healthy foods like leafy greens, nuts, and fatty fish rich in omega-3s.
While the link between gum disease and heart health is compelling, it’s not deterministic. Not everyone with gum disease will develop cardiovascular issues, but the risk is significant enough to warrant proactive measures. Think of oral care as a preventive strategy for heart health, much like managing cholesterol or blood pressure. By addressing gum disease early, you’re not just saving your teeth—you’re potentially safeguarding your heart. This dual benefit makes oral hygiene an indispensable part of overall wellness.
Understanding Gum Disease Progression: How Quickly Can It Advance?
You may want to see also

Systemic Infections: How gum disease can lead to severe systemic infections if left untreated
Gum disease, if neglected, can become a silent gateway for systemic infections that affect far more than your mouth. Periodontitis, the advanced form of gum disease, allows harmful bacteria to infiltrate the bloodstream through inflamed or bleeding gums. Once in the circulatory system, these pathogens can travel to vital organs, triggering infections that range from severe to life-threatening. For instance, oral bacteria like *Porphyromonas gingivalis* have been detected in atherosclerotic plaques, suggesting a direct link to cardiovascular complications. This isn’t just a theoretical risk—it’s a documented pathway for conditions like endocarditis, pneumonia, and even sepsis.
Consider the mechanics of this progression. When plaque builds up and hardens into tartar, it creates a breeding ground for bacteria that produce toxins. These toxins irritate the gums, causing them to pull away from the teeth and form pockets that harbor more bacteria. Over time, the body’s immune response to this chronic infection can lead to systemic inflammation. For adults over 65 or individuals with compromised immune systems, this process accelerates, increasing susceptibility to infections like bacterial pneumonia, which occurs when oral bacteria are aspirated into the lungs. Practical prevention includes twice-daily brushing with fluoride toothpaste, flossing, and regular dental check-ups every six months.
The connection between gum disease and systemic infections isn’t just correlational—it’s causal. Research shows that treating periodontitis can reduce markers of systemic inflammation, such as C-reactive protein levels, by up to 30%. Conversely, untreated gum disease elevates the risk of complications like diabetic complications, as inflammation interferes with insulin sensitivity. Pregnant individuals should also take note: periodontal disease is linked to preterm birth and low birth weight, likely due to the systemic inflammatory response. To mitigate these risks, incorporate antimicrobial mouthwashes containing chlorhexidine (0.12% concentration) into your oral care routine, especially if you’re at higher risk.
A comparative analysis highlights the urgency of addressing gum disease. While a cavity is a localized issue, periodontitis is a systemic threat. For example, a study in the *Journal of Periodontology* found that individuals with severe gum disease are twice as likely to develop respiratory infections compared to those with healthy gums. Similarly, the risk of cardiovascular events, such as stroke or heart attack, increases by 20% in the presence of untreated periodontitis. These statistics underscore the importance of viewing oral health as inseparable from overall health. If you notice symptoms like persistent bad breath, bleeding gums, or loose teeth, seek dental care immediately—delaying treatment could have far-reaching consequences.
Finally, consider the economic and personal toll of ignoring gum disease. Hospitalizations for systemic infections linked to poor oral health cost the U.S. healthcare system billions annually. Yet, preventive measures are remarkably cost-effective. A professional dental cleaning costs around $100–$200, while treating sepsis can exceed $50,000. Beyond finances, the impact on quality of life is profound. Systemic infections can lead to chronic fatigue, organ damage, and even disability. By prioritizing oral hygiene and addressing gum disease early, you’re not just saving teeth—you’re safeguarding your entire body. Remember, the mouth is the body’s gateway; keep it healthy to protect what lies beyond.
Apple Cider Vinegar Remedies for Gum Disease: A Natural Guide
You may want to see also

Diabetes Complications: Impact of gum disease on diabetes management and overall health risks
Gum disease, or periodontal disease, is more than just a dental issue—it’s a silent disruptor of systemic health, particularly for individuals with diabetes. Research shows that the relationship between gum disease and diabetes is bidirectional: not only does diabetes increase the risk of gum disease, but untreated gum disease can also exacerbate diabetes management. This vicious cycle highlights why addressing oral health is critical for anyone managing diabetes.
Consider this: elevated blood sugar levels create an ideal environment for bacteria to thrive in the mouth, leading to gum inflammation and infection. Simultaneously, gum disease triggers an inflammatory response that can interfere with insulin’s effectiveness, making blood sugar control more challenging. For instance, a study published in *Diabetes Care* found that individuals with severe gum disease had higher HbA1c levels, a key marker of long-term blood sugar control. This means poor oral health can directly undermine diabetes management efforts, increasing the risk of complications like nerve damage, kidney disease, and cardiovascular issues.
Practical steps to mitigate this risk include maintaining a rigorous oral hygiene routine: brushing twice daily with fluoride toothpaste, flossing daily, and using an antimicrobial mouthwash. Diabetic individuals should also schedule dental check-ups every six months or more frequently if recommended by their dentist. For those with advanced gum disease, professional treatments like scaling and root planing can help manage the condition. Additionally, keeping blood sugar levels within target ranges—typically 70–130 mg/dL before meals and less than 180 mg/dL two hours after meals—can reduce the risk of gum disease progression.
A comparative analysis reveals that diabetic patients with well-managed oral health are less likely to experience severe diabetes complications. For example, a longitudinal study in *The Journal of Clinical Periodontology* demonstrated that treating gum disease in diabetic patients led to a 0.4% reduction in HbA1c levels, equivalent to the effect of adding a new diabetes medication. This underscores the importance of integrating oral care into diabetes management plans.
In conclusion, gum disease isn’t just a dental problem—it’s a significant threat to diabetes control and overall health. By prioritizing oral hygiene and regular dental care, individuals with diabetes can break the cycle of inflammation and insulin resistance, reducing their risk of life-threatening complications. Remember, a healthy mouth is a cornerstone of a healthy body, especially when managing chronic conditions like diabetes.
Recognizing Early Signs of Periodontal Disease: Symptoms and Prevention Tips
You may want to see also

Respiratory Problems: Connection between gum disease and respiratory conditions like pneumonia
Gum disease, often dismissed as a mere oral health issue, can have far-reaching consequences, including a surprising link to respiratory conditions like pneumonia. The mouth is a gateway to the respiratory system, and poor oral hygiene allows harmful bacteria to travel from the gums into the lungs, exacerbating or even causing respiratory infections. This connection is particularly alarming for vulnerable populations, such as the elderly, immunocompromised individuals, and those with chronic lung diseases like COPD.
Consider the mechanism: when gum disease progresses, it creates an environment where bacteria thrive. These pathogens can be aspirated into the lungs, leading to infections like pneumonia. Studies have shown that individuals with severe gum disease (periodontitis) are at a significantly higher risk of developing respiratory infections. For instance, a 2019 study published in the *Journal of Periodontology* found that patients with periodontitis had a 1.7 times greater risk of pneumonia compared to those with healthy gums. This highlights the critical need for oral care as a preventive measure against respiratory complications.
To mitigate this risk, practical steps can be taken. First, maintain rigorous oral hygiene: brush twice daily with fluoride toothpaste, floss daily, and use an antimicrobial mouthwash. Regular dental check-ups are essential, especially for those over 60 or with pre-existing health conditions. For individuals with chronic lung diseases, dentists may recommend more frequent cleanings to reduce bacterial buildup. Additionally, staying hydrated and avoiding smoking can significantly lower the risk of both gum disease and respiratory infections.
A comparative analysis reveals that the link between gum disease and pneumonia is not just correlational but causal. Bacterial strains like *Porphyromonas gingivalis*, commonly found in periodontitis patients, have been isolated in lung tissue samples of pneumonia patients. This underscores the importance of treating gum disease not just as an oral issue but as a systemic health concern. For healthcare providers, integrating oral health assessments into routine care for respiratory patients could be a game-changer in preventing complications.
In conclusion, the connection between gum disease and respiratory conditions like pneumonia is a stark reminder of the body’s interconnectedness. By prioritizing oral health, individuals can reduce their risk of life-threatening respiratory infections. This is not merely about brushing and flossing—it’s about adopting a holistic approach to health that recognizes the mouth as a vital component of overall well-being. Ignoring gum disease could indeed have fatal consequences, making proactive care an essential, not optional, practice.
Reversing Gum Disease: Understanding the Timeline for Healthy Gums
You may want to see also

Cancer Risks: Studies suggesting a potential link between gum disease and certain cancers
Gum disease, a prevalent oral health issue, has long been associated with systemic health problems, but its potential link to cancer is a growing area of research. Recent studies suggest that the chronic inflammation and bacterial infections characteristic of gum disease may contribute to the development of certain cancers. For instance, research published in the *Journal of the National Cancer Institute* found that individuals with severe gum disease had a 24% higher risk of developing lung cancer and a 13% higher risk of colorectal cancer compared to those with healthy gums. These findings underscore the importance of oral health as a potential modifiable risk factor for cancer prevention.
Analyzing the mechanisms behind this link reveals a complex interplay between oral bacteria and systemic inflammation. *Porphyromonas gingivalis*, a key bacterium in gum disease, has been detected in cancerous tissues, suggesting it may play a role in tumorigenesis. Additionally, chronic inflammation, a hallmark of gum disease, can promote DNA damage and cell proliferation, both of which are critical steps in cancer development. For example, elevated levels of inflammatory markers like C-reactive protein (CRP) in gum disease patients have been correlated with increased cancer risk. This biological connection highlights the need for proactive oral care as part of a broader cancer prevention strategy.
Practical steps to mitigate these risks include maintaining rigorous oral hygiene practices, such as brushing twice daily with fluoride toothpaste and flossing daily. Regular dental check-ups are essential, particularly for individuals over 45, as gum disease prevalence increases with age. For those with existing gum disease, professional treatments like scaling and root planing can reduce bacterial load and inflammation. Incorporating anti-inflammatory foods, such as leafy greens and fatty fish, into the diet may also help manage systemic inflammation. These measures not only protect oral health but could potentially reduce the risk of cancer associated with gum disease.
Comparatively, the link between gum disease and cancer is not as well-established as other risk factors like smoking or obesity, but emerging evidence warrants attention. For example, while smoking increases lung cancer risk by 2,500%, the 24% increase associated with gum disease is still significant, especially considering its prevalence. Unlike smoking, gum disease is often reversible, making it a more actionable target for intervention. Public health initiatives should emphasize this connection, encouraging individuals to prioritize oral health as a component of overall cancer prevention.
In conclusion, the potential link between gum disease and certain cancers adds a critical dimension to the question, "Will gum disease kill you?" While not a direct cause of death, its association with increased cancer risk highlights the systemic impact of oral health. By understanding this connection and taking proactive steps to prevent and treat gum disease, individuals can potentially reduce their cancer risk and improve overall health. This emerging research serves as a reminder that oral care is not just about preserving teeth—it’s about safeguarding your entire well-being.
Effective Home Remedies to Treat Gum Disease Without Dental Visits
You may want to see also
Frequently asked questions
Gum disease itself is not directly fatal, but severe cases, such as advanced periodontitis, can lead to serious health complications like heart disease, diabetes complications, and respiratory infections, which may increase the risk of mortality.
Gum disease is linked to systemic inflammation, which can exacerbate conditions like cardiovascular disease, stroke, and diabetes. Poor oral health can reduce quality of life and indirectly contribute to a shorter lifespan if left untreated.
Yes, maintaining good oral hygiene (brushing, flossing, and regular dental check-ups) can prevent gum disease. Early treatment of gum issues and managing associated health conditions can significantly reduce the risk of complications.