Tooth implants are a popular and effective solution for replacing missing teeth, offering a permanent and natural-looking restoration. However, circumstances may arise where a patient or dentist considers removing an implant, such as infection, implant failure, or changes in the patient's oral health. While implants are designed to be a long-term solution, they are not always irreversible, and removal is possible, albeit with careful consideration and planning. The process of removing a tooth implant, known as explantation, requires a skilled dental professional and may involve surgical intervention, depending on the implant's integration with the surrounding bone and tissue. Understanding the reasons for and implications of implant removal is essential for patients and dentists alike to make informed decisions about oral health and treatment options.
| Characteristics | Values |
|---|---|
| Can a tooth implant be removed? | Yes, dental implants can be removed if necessary. |
| Reasons for removal | Infection, implant failure, nerve damage, patient request, or complications. |
| Removal procedure | Surgical procedure performed by a dentist or oral surgeon. |
| Anesthesia | Local anesthesia is typically used during the removal process. |
| Recovery time | Varies, but typically a few days to a week for initial healing. |
| Success rate of removal | High, with minimal risks when performed by an experienced professional. |
| Potential risks | Bleeding, infection, damage to surrounding teeth or tissues. |
| Cost of removal | Varies by location and complexity, but generally ranges from $1,000 to $3,000. |
| Replacement options | After removal, a new implant, bridge, or denture can be considered. |
| Long-term impact | Removal may require additional procedures to restore function and aesthetics. |
What You'll Learn
- Reasons for Removal: Infection, nerve damage, or implant failure may necessitate removal of a tooth implant
- Removal Procedure: A surgical process to extract the implant, often under local anesthesia
- Recovery Time: Healing typically takes 1-2 weeks, with full recovery in 3-6 months
- Cost of Removal: Expenses vary, depending on complexity and location, ranging from $200 to $2,000
- Alternatives to Removal: Bone grafting, crown replacement, or antibiotic treatment may resolve issues without extraction

Reasons for Removal: Infection, nerve damage, or implant failure may necessitate removal of a tooth implant
Tooth implants, while highly successful, are not immune to complications. Among the most critical reasons for their removal are infection, nerve damage, and implant failure. These issues, though relatively rare, demand immediate attention to prevent further oral health deterioration. Understanding these risks underscores the importance of regular dental check-ups and prompt intervention when symptoms arise.
Infection, often referred to as peri-implantitis, is a leading cause for implant removal. This condition occurs when bacteria infiltrate the gum tissue surrounding the implant, leading to inflammation, bone loss, and eventual instability. Symptoms include persistent pain, swelling, and pus discharge. Treatment typically begins with antibiotics, but if the infection persists or recurs, removal may be the only option to prevent systemic health risks. Patients with compromised immune systems, such as diabetics or smokers, are particularly vulnerable and should adhere strictly to post-implant care protocols.
Nerve damage is another serious complication that may necessitate implant removal. During placement, proximity to the inferior alveolar nerve (in the lower jaw) or other neural structures poses a risk of injury. Symptoms include numbness, tingling, or persistent pain in the lips, chin, or tongue. While rare, such damage can be irreversible, and removing the implant may be essential to prevent long-term sensory impairment. Dentists often use advanced imaging techniques like cone-beam CT scans to minimize this risk during planning, but it remains a critical consideration.
Implant failure, though uncommon, can occur due to factors like poor osseointegration (fusion with the jawbone), mechanical overload, or material defects. Signs of failure include mobility, discomfort, or visible exposure of the implant. In such cases, removal is often followed by a waiting period to allow the site to heal before attempting a new implant or exploring alternative tooth replacement options. Patients with conditions like osteoporosis or those taking bisphosphonates are at higher risk and should discuss these factors with their dentist beforehand.
While the prospect of removal is unsettling, it is a testament to the body’s protective mechanisms and the importance of addressing complications early. Dentists prioritize preserving implants whenever possible, but when infection, nerve damage, or failure occur, removal becomes a necessary step toward restoring oral health. Patients should remain vigilant for warning signs and maintain open communication with their dental provider to ensure the best possible outcomes.
Can Retainers Cause Tooth Death? Understanding the Risks of Tight Wear
You may want to see also

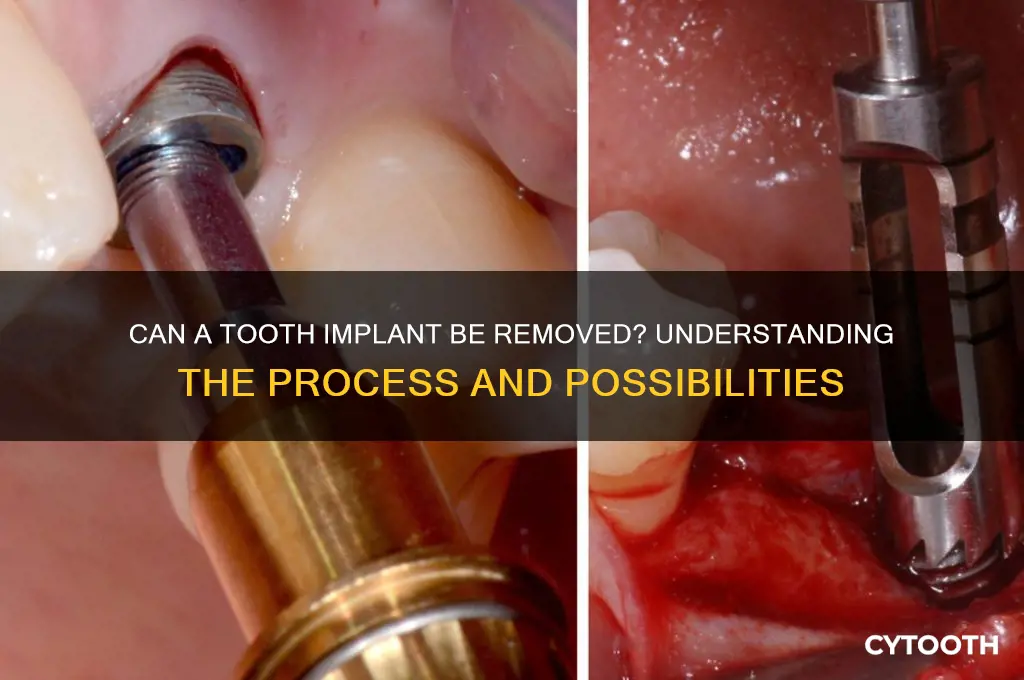
Removal Procedure: A surgical process to extract the implant, often under local anesthesia
Tooth implants, while designed for longevity, are not always permanent fixtures. The removal procedure is a surgical process that requires precision and care, typically performed under local anesthesia to ensure patient comfort. This process is not as straightforward as extracting a natural tooth, given the implant’s integration with the jawbone. The surgeon begins by making an incision in the gum tissue to expose the implant, followed by the careful detachment of any bone that has fused to the implant surface. Specialized tools, such as reverse torque ratchets, are used to unscrew the implant from its position without causing excessive trauma to the surrounding bone. The complexity of this step depends on factors like the implant’s age, the quality of osseointegration, and the patient’s bone density.
Post-removal, the site requires meticulous management to promote healing and prevent complications. The surgeon may opt to place a bone graft if significant bone loss is evident, ensuring the socket can support future restorative options. Antibiotics are often prescribed to mitigate infection risk, particularly in cases where the implant was removed due to peri-implantitis. Patients are advised to follow a soft diet for several days and avoid strenuous activities to minimize swelling and bleeding. Pain management typically involves over-the-counter analgesics like ibuprofen (600–800 mg every 6–8 hours) or acetaminophen (500–1000 mg every 4–6 hours), though stronger prescriptions may be provided for more invasive cases.
The decision to remove an implant is rarely taken lightly, as it involves weighing the risks of surgery against the benefits of resolution. Common reasons for removal include implant failure, persistent infection, or the need to address poor positioning. For instance, implants placed too close to vital structures like the inferior alveolar nerve may require extraction to prevent long-term complications. Comparative studies show that implants with surface contamination or those placed in smokers have higher failure rates, making removal more likely in these populations. Understanding these factors helps both clinicians and patients make informed decisions about whether removal is the best course of action.
From a practical standpoint, patients should be aware that the removal procedure is not a quick fix but a deliberate process aimed at preserving oral health. Recovery times vary, with initial healing taking 1–2 weeks, though complete bone regeneration can take 3–6 months. During this period, patients may experience discomfort, swelling, and minor bleeding, which can be managed with cold compresses and proper oral hygiene. A follow-up appointment is crucial to assess healing and discuss potential replacement options, such as a new implant, bridge, or denture. By approaching the removal procedure with clarity and preparation, patients can navigate this challenging process with greater confidence and understanding.
Sore Tooth, Headache Connection: Understanding the Surprising Link
You may want to see also

Recovery Time: Healing typically takes 1-2 weeks, with full recovery in 3-6 months
The initial healing phase after a tooth implant removal is surprisingly swift, typically spanning just 1-2 weeks. During this period, the focus is on managing discomfort and preventing infection. Patients are often prescribed a course of antibiotics, such as amoxicillin (500 mg, three times daily for 7 days), to ward off bacterial invasion of the exposed socket. Pain management is equally crucial, with over-the-counter medications like ibuprofen (600 mg every 6 hours) or acetaminophen (1000 mg every 8 hours) recommended to alleviate soreness. It’s essential to follow the dentist’s instructions meticulously, including avoiding strenuous activities and sticking to a soft diet to minimize stress on the healing site.
Beyond the initial two weeks, the body enters a more gradual phase of recovery, which can extend from 3 to 6 months. This period is marked by osseous integration, where the surrounding bone remodels and strengthens around the extraction site. Patients should be aware that this stage is less about symptom management and more about fostering optimal healing. Calcium and vitamin D supplements (1000 mg and 800 IU daily, respectively) can support bone health, though consultation with a healthcare provider is advised to tailor dosages. Regular follow-ups with the dentist are critical to monitor progress and address any complications, such as dry socket or delayed healing.
Comparatively, the recovery timeline for implant removal is often shorter than that of implant placement, which requires osseointegration of a foreign object. However, the removal process can still introduce variables that affect healing, such as the complexity of the extraction or the patient’s overall health. Smokers, for instance, may experience prolonged recovery due to impaired blood flow, while individuals with diabetes or autoimmune disorders might face heightened infection risks. These factors underscore the importance of personalized care plans and proactive health management during recovery.
Practically, patients can expedite healing by adhering to specific post-removal guidelines. Rinsing with a warm saline solution (1/2 teaspoon of salt in 8 ounces of water) 2-3 times daily can keep the area clean without irritating the tissues. Avoiding smoking and alcohol is non-negotiable, as both can delay healing and increase infection risk. Additionally, maintaining excellent oral hygiene—gently brushing around the extraction site and using interdental brushes to clean adjacent teeth—prevents plaque buildup that could compromise recovery. By combining medical adherence with these practical measures, patients can navigate the recovery process with greater ease and confidence.
Saving a Cracked Tooth Under a Crown: Is It Possible?
You may want to see also

Cost of Removal: Expenses vary, depending on complexity and location, ranging from $200 to $2,000
The cost of removing a tooth implant is not a one-size-fits-all figure. It’s a spectrum, influenced by factors like the implant’s location, the complexity of the procedure, and even your geographic area. Prices can range dramatically, from as low as $200 to as high as $2,000, making it essential to understand what drives these variations. For instance, a straightforward removal in a rural area might lean toward the lower end, while a complicated extraction in a major city could push costs upward due to higher overhead and specialized care.
Consider the process itself. If the implant is easily accessible and hasn’t integrated deeply with the jawbone, removal may be quick and minimally invasive, keeping costs closer to the $200 mark. However, if the implant has fused extensively with the bone or is located in a hard-to-reach area, such as the rear molars, the procedure becomes more intricate. This might require advanced techniques, additional anesthesia, or even a referral to an oral surgeon, significantly increasing the expense. For example, a posterior implant removal could easily approach the $1,000 range due to the precision and time involved.
Location plays a pivotal role in pricing as well. In metropolitan areas, where the cost of living and operating a dental practice is higher, patients often face steeper fees. Conversely, in smaller towns or regions with lower living costs, the same procedure might be more affordable. It’s not uncommon for patients to travel to nearby cities or states to find more competitive pricing, though this approach requires weighing the savings against travel and potential follow-up care expenses.
Before committing to removal, it’s crucial to consult with your dentist or oral surgeon for a detailed cost breakdown. Ask about all potential fees, including pre-operative exams, anesthesia, and post-removal care. Some practices offer payment plans or financing options, which can make the expense more manageable. Additionally, check your dental insurance policy—while many plans don’t cover implant removal, some may provide partial coverage for medically necessary procedures. Understanding these nuances can help you navigate the financial aspect with greater confidence.
Ultimately, the cost of removing a tooth implant is a balancing act between necessity and affordability. While the price tag can be daunting, especially at the higher end of the spectrum, it’s often a worthwhile investment in oral health and comfort. By researching thoroughly, discussing options with your provider, and exploring financial assistance, you can make an informed decision that aligns with both your health needs and your budget.
Fixing a Broken Tooth with a Filling: Repair Options Explained
You may want to see also

Alternatives to Removal: Bone grafting, crown replacement, or antibiotic treatment may resolve issues without extraction
Tooth implant complications don’t always require removal. Bone grafting, for instance, can address issues like implant instability or bone loss by regenerating the jawbone structure. This procedure involves transplanting bone material—either from another part of your body (autograft), a donor (allograft), or synthetic sources—to the affected area. Post-surgery, patients typically need 3–6 months for the graft to integrate fully, followed by implant re-evaluation. Success rates for bone grafting in implant salvage range from 85% to 95%, making it a viable alternative to extraction.
Crown replacement offers another non-invasive solution, particularly for issues like wear, fracture, or aesthetic dissatisfaction. Modern crowns, crafted from materials like zirconia or porcelain, are designed to mimic natural teeth and withstand biting forces. The process involves removing the existing crown, preparing the implant abutment, and attaching a new restoration—often completed in 2–3 appointments. For patients with peri-implantitis, replacing the crown can also improve oral hygiene access, reducing bacterial buildup around the implant.
Antibiotic treatment serves as a targeted approach for infections like peri-implantitis, which threaten implant stability. Systemic antibiotics such as amoxicillin (500 mg, 3 times daily for 7–10 days) or metronidazole (250 mg, 3 times daily) are commonly prescribed, often paired with local antimicrobial rinses like chlorhexidine (0.12%). For severe cases, a combination of surgical debridement and antibiotic therapy may be necessary. While antibiotics alone cannot resolve structural issues, they can halt infection progression, preserving the implant and surrounding bone.
Comparing these alternatives, bone grafting is most effective for structural deficiencies but requires significant healing time. Crown replacement is quick and minimally invasive, ideal for cosmetic or functional issues. Antibiotic treatment is best for infections but must be paired with proper oral hygiene to prevent recurrence. Each option underscores the principle that removal should be a last resort, with tailored interventions often resolving implant complications effectively.
Can a Bad Tooth Cause Dizziness? Exploring the Surprising Connection
You may want to see also
Frequently asked questions
Yes, a tooth implant can be removed if it becomes infected, damaged, or fails to integrate properly. The process involves a surgical procedure to extract the implant, followed by healing and potential replacement if desired.
The removal of a tooth implant is typically performed under local anesthesia, so the procedure itself is not painful. Post-operative discomfort can be managed with pain medication, and the level of pain varies depending on the complexity of the removal.
Yes, after a tooth implant is removed and the site has healed, it is often possible to place a new implant. However, the success of the new implant depends on factors like bone health, the reason for the original implant's removal, and proper planning by the dental professional.

















