A sore tooth can indeed contribute to headaches, as the pain often radiates to surrounding areas due to shared nerve pathways. Dental issues such as cavities, infections, or gum disease can trigger referred pain, causing discomfort in the head, temples, or jaw. This occurs because the trigeminal nerve, which innervates the face and mouth, also connects to headache-sensitive areas. Additionally, tooth pain can lead to tension in the facial and neck muscles, further exacerbating headache symptoms. Understanding this connection is crucial for identifying the root cause of headaches and seeking appropriate dental or medical treatment.
| Characteristics | Values |
|---|---|
| Connection Between Tooth Pain and Headache | Yes, a sore tooth can cause headaches due to shared nerve pathways. |
| Mechanism | Trigeminal nerve (cranial nerve V) innervates both teeth and head regions. |
| Types of Headaches | Tension headaches, migraines, or referred pain in the temple or jaw area. |
| Common Causes | Tooth decay, infection (abscess), gum disease, or TMJ disorders. |
| Symptoms | Toothache, throbbing pain, sensitivity, radiating pain to head or jaw. |
| Treatment | Dental intervention (fillings, root canals), pain relievers, or antibiotics. |
| Prevention | Regular dental check-ups, good oral hygiene, and addressing dental issues promptly. |
| When to See a Dentist | Persistent tooth pain, swelling, fever, or severe headache. |
| Related Conditions | Sinus infections, bruxism (teeth grinding), or neuralgia. |
| Medical Consensus | Widely recognized by dental and medical professionals as a possible cause. |
What You'll Learn
- Referred Pain Mechanisms: How tooth pain can radiate to head due to shared nerve pathways
- Sinus Pressure Link: Tooth infections causing sinus inflammation, leading to headache symptoms
- TMJ Strain: Toothaches triggering jaw tension, resulting in headache or migraine-like pain
- Inflammation Spread: Localized tooth inflammation affecting nearby tissues, causing head discomfort
- Stress and Tension: Tooth pain inducing muscle tension in head and neck areas

Referred Pain Mechanisms: How tooth pain can radiate to head due to shared nerve pathways
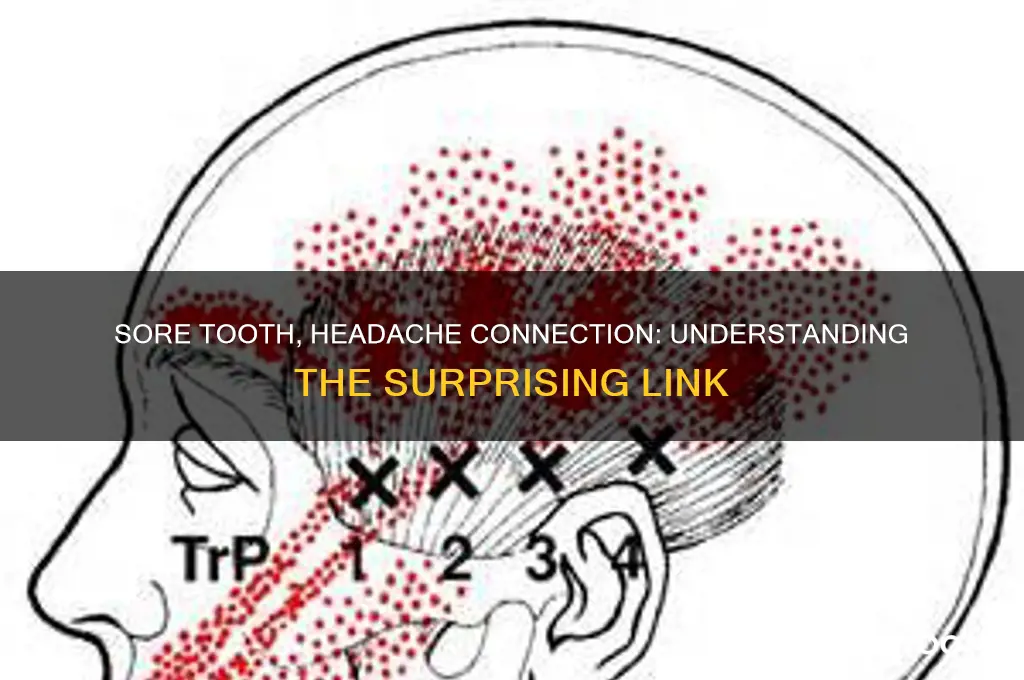
Tooth pain can indeed radiate to the head, a phenomenon rooted in the intricate network of shared nerve pathways. The trigeminal nerve, one of the largest nerves in the head, plays a central role in this process. It branches into three divisions, one of which innervates the teeth and gums. When inflammation or infection occurs in a tooth, the trigeminal nerve signals pain, but these signals can sometimes be misinterpreted by the brain. This miscommunication leads to referred pain, where the brain perceives the discomfort as originating from a different location, such as the head, rather than the tooth itself.
Understanding this mechanism is crucial for accurate diagnosis and treatment. For instance, a patient complaining of a persistent headache might actually be experiencing a dental issue. Dentists and healthcare providers often rely on detailed patient histories and targeted examinations to trace the pain back to its source. A common example is a sinus infection or impacted wisdom tooth, where the pain can mimic tension headaches or migraines. Recognizing these patterns can prevent unnecessary treatments and ensure the underlying dental problem is addressed promptly.
From a practical standpoint, managing referred tooth pain involves both immediate relief and long-term care. Over-the-counter pain relievers like ibuprofen (200–400 mg every 4–6 hours) can temporarily alleviate symptoms, but they do not address the root cause. Cold compresses applied to the affected area for 15–20 minutes at a time can reduce inflammation and numb the pain. However, persistent or severe symptoms warrant a dental evaluation. A dentist may recommend procedures such as root canal therapy, extraction, or antibiotics, depending on the cause of the tooth pain.
Comparatively, referred pain from dental issues differs from primary headaches in its origin and treatment. While migraines or tension headaches often respond to medications like triptans or lifestyle changes, tooth-related headaches require dental intervention. For example, a cracked tooth or abscess can cause pain that radiates to the temple or jaw, mimicking a sinus headache. Distinguishing between these conditions involves assessing factors like pain triggers (e.g., chewing or temperature sensitivity) and accompanying symptoms (e.g., tooth sensitivity or bad taste in the mouth).
In conclusion, referred pain mechanisms highlight the interconnectedness of the body’s sensory systems. By understanding how tooth pain can radiate to the head via shared nerve pathways, individuals can take proactive steps to identify and address the underlying issue. Regular dental check-ups, prompt attention to oral discomfort, and collaboration between healthcare providers are key to managing this often-overlooked connection between dental health and headaches.
Fixing a Broken Tooth with a Filling: Repair Options Explained
You may want to see also

Sinus Pressure Link: Tooth infections causing sinus inflammation, leading to headache symptoms
Tooth infections, particularly those affecting the upper molars, can silently trigger a cascade of sinus issues that culminate in headache symptoms. The maxillary sinuses sit just above the roots of these teeth, separated only by a thin layer of bone. When bacteria from an infected tooth breach this barrier, they can inflame the sinus lining, causing pressure and pain that radiates to the forehead, temples, or behind the eyes. This overlap in symptoms often leads individuals to mistake a dental problem for a sinus headache or migraine, delaying proper treatment.
Consider the anatomy: the proximity of the maxillary sinuses to the upper teeth means even minor dental infections can have outsized consequences. For instance, a persistent toothache in the upper jaw might not only be a localized issue but a precursor to sinusitis. Symptoms such as facial tenderness, nasal congestion, and headache often emerge as the infection spreads, mimicking classic sinus headache patterns. Recognizing this connection is crucial, as treating the tooth infection—whether through root canal therapy, antibiotics, or extraction—can resolve both the dental pain and the associated sinus pressure.
From a practical standpoint, distinguishing between a sinus headache and one caused by a tooth infection requires attention to detail. Key indicators include the presence of dental pain, sensitivity to temperature, or visible swelling around the affected tooth. If these signs accompany headache symptoms, especially in the upper facial region, a dental evaluation should be prioritized. Over-the-counter pain relievers like ibuprofen (400–600 mg every 6 hours) may provide temporary relief, but they do not address the underlying infection. Nasal decongestants or saline rinses can alleviate sinus pressure, but they are merely adjunctive measures.
A comparative analysis highlights the importance of early intervention. Untreated tooth infections can lead to chronic sinusitis, abscess formation, or even systemic complications like sepsis. Conversely, timely dental treatment not only eliminates the source of infection but also prevents the progression of sinus inflammation. For adults over 18, a dental checkup every six months can catch issues before they escalate, while children and adolescents should follow their dentist’s recommendations based on oral health status.
In conclusion, the sinus pressure link between tooth infections and headaches underscores the interconnectedness of oral and sinus health. By understanding this relationship, individuals can take proactive steps to address symptoms at their root cause. Whether through regular dental care, prompt treatment of infections, or collaboration between dentists and ENT specialists, breaking the cycle of tooth-related sinus headaches is both achievable and essential for long-term well-being.
Can a Bad Tooth Cause Dizziness? Exploring the Surprising Connection
You may want to see also

TMJ Strain: Toothaches triggering jaw tension, resulting in headache or migraine-like pain
A sore tooth can indeed trigger a cascade of discomfort that extends far beyond the mouth, often culminating in headaches or migraine-like pain. This phenomenon is frequently linked to TMJ (temporomandibular joint) strain, a condition where the jaw joint becomes overworked or misaligned. When a toothache occurs, the natural tendency to favor the unaffected side or clench the jaw in response to pain can place undue stress on the TMJ. Over time, this tension radiates to surrounding muscles, particularly the temples and neck, leading to headache symptoms. Understanding this connection is crucial for anyone experiencing persistent head pain alongside dental issues.
Consider the mechanics: the TMJ acts as a hinge connecting the jawbone to the skull, facilitating movements like chewing and speaking. When a toothache disrupts normal chewing patterns, the jaw compensates by overworking the joint. For instance, grinding teeth or clenching the jaw—common reactions to dental pain—can exacerbate TMJ strain. This tension doesn’t remain localized; it travels along the trigeminal nerve, which supplies sensation to the face and is closely linked to headache pathways. As a result, what starts as a toothache can manifest as a throbbing headache or even migraine-like symptoms, such as sensitivity to light or sound.
To alleviate TMJ-related headaches, start with targeted self-care measures. Applying a warm compress to the jaw for 10–15 minutes can relax tense muscles, while gentle jaw stretches—opening and closing the mouth slowly or moving the jaw side to side—can improve mobility. Over-the-counter anti-inflammatory medications like ibuprofen (200–400 mg every 4–6 hours) can reduce both toothache pain and associated inflammation in the TMJ. For nighttime relief, consider a mouthguard to prevent clenching or grinding, which is especially common in adults aged 20–40. However, avoid excessive gum chewing or hard foods that strain the jaw further.
While self-care is effective for mild cases, persistent symptoms warrant professional intervention. A dentist can address the underlying toothache, possibly through a root canal or extraction, while a physical therapist specializing in TMJ disorders can provide tailored exercises to strengthen jaw muscles. In severe cases, a dentist might recommend a splint or orthodontic adjustments to correct misalignment. Ignoring TMJ strain can lead to chronic headaches, so early intervention is key. By treating the root cause—the toothache—and managing jaw tension, individuals can break the cycle of pain and restore comfort.
Finally, prevention plays a vital role in avoiding TMJ strain and its headache consequences. Maintain good oral hygiene to prevent toothaches, and be mindful of habits like nail-biting or excessive gum chewing that strain the jaw. Stress management techniques, such as mindfulness or progressive muscle relaxation, can reduce clenching tendencies. For those with a history of TMJ issues, regular dental check-ups are essential to monitor jaw health. By addressing both dental and jaw concerns proactively, individuals can minimize the risk of headaches and maintain overall well-being.
Saving a Cracked Tooth Under a Crown: Is It Possible?
You may want to see also

Inflammation Spread: Localized tooth inflammation affecting nearby tissues, causing head discomfort
Tooth inflammation, often stemming from infection or decay, doesn’t remain isolated. The maxillary sinuses, for instance, sit directly above the upper molars, separated only by a thin layer of bone. When a tooth becomes infected, bacteria and inflammatory mediators can spread to these sinuses, triggering sinusitis. This proximity explains why a sore tooth can lead to facial pressure, pain, and headaches, particularly in the forehead or cheekbones. Understanding this anatomical connection is crucial for recognizing the root cause of head discomfort.
Consider the trigeminal nerve, the body’s largest cranial nerve, which innervates the face, teeth, and jaw. Inflammation in a tooth can irritate this nerve, causing referred pain that radiates to the head. This phenomenon, known as trigeminal neuralgia, often manifests as sharp, shooting headaches or migraines. For example, a decaying lower molar might cause pain that feels like it’s originating from the temple or behind the eye. Identifying this nerve involvement is key to distinguishing dental-related headaches from other types.
To mitigate inflammation spread, early intervention is essential. Rinsing with warm saltwater (1/2 teaspoon of salt in 8 ounces of water) can reduce bacterial load and soothe irritated tissues. Over-the-counter anti-inflammatory medications like ibuprofen (200–400 mg every 6 hours) can alleviate pain and swelling, but they’re not a long-term solution. For persistent cases, a dentist may prescribe antibiotics (e.g., amoxicillin 500 mg three times daily for adults) to target the infection. Ignoring these symptoms risks further complications, such as abscess formation or systemic infection.
Comparatively, while tension headaches often stem from muscle strain, dental-related headaches are rooted in inflammation and nerve irritation. A key differentiator is the presence of dental symptoms like sensitivity to hot or cold, gum swelling, or a persistent bad taste. Keeping a symptom journal can help track patterns—note when tooth pain coincides with headaches, as this correlation is a red flag. Addressing the dental issue directly, such as through a root canal or extraction, often resolves both the toothache and associated head discomfort.
Finally, preventive measures are paramount. Regular dental check-ups every six months can catch decay or infection before it spreads. For those prone to cavities, fluoride treatments or dental sealants can provide an extra layer of protection. At home, maintaining oral hygiene with twice-daily brushing, flossing, and an antimicrobial mouthwash reduces the risk of inflammation. By addressing localized tooth issues promptly, you can prevent the discomfort from escalating into a full-blown headache, ensuring both dental and cranial health remain intact.

Stress and Tension: Tooth pain inducing muscle tension in head and neck areas
Tooth pain rarely stays localized; it has a knack for radiating discomfort far beyond the affected area. One surprising consequence? Increased muscle tension in the head and neck. When a toothache persists, the body’s natural response is to clench the jaw or tighten surrounding muscles as a protective reflex. Over time, this chronic tension can trigger headaches, particularly tension-type headaches, which feel like a tight band around the head. The trigeminal nerve, responsible for facial and oral sensations, plays a key role here—its irritation from tooth pain can send stress signals to nearby muscles, creating a cycle of discomfort.
Consider this scenario: a 35-year-old professional with an untreated cavity experiences recurring tooth pain. Unconsciously, they clench their jaw during sleep or while concentrating at work. Within weeks, they notice frequent headaches originating at the temples and radiating to the neck. This isn’t coincidence—it’s biomechanics. Prolonged muscle tension reduces blood flow to the head and neck, causing ischemia (lack of oxygen) in tissues, which manifests as headache pain. Even children, aged 10–15, with orthodontic discomfort or wisdom tooth eruption can exhibit similar symptoms, though their headaches may be shorter in duration due to less developed muscle patterns.
Breaking this cycle requires a two-pronged approach. First, address the root cause: the tooth pain. A dental evaluation might reveal issues like cavities, abscesses, or bruxism (teeth grinding), often exacerbated by stress. Treatment could range from fillings to root canals, depending on severity. Second, manage the muscle tension. Applying a warm compress to the jaw for 10–15 minutes twice daily can relax the temporomandibular joint (TMJ). Gentle neck stretches—like tilting the ear to the shoulder and holding for 20 seconds—can alleviate tightness. For persistent cases, a physical therapist might recommend exercises to strengthen postural muscles, reducing strain on the head and neck.
A cautionary note: over-the-counter pain relievers like ibuprofen (400–600 mg every 6 hours) can temporarily ease symptoms but don’t address the underlying issue. Relying solely on medication risks masking a worsening dental problem. Similarly, while stress-reduction techniques like mindfulness or progressive muscle relaxation can help, they’re adjuncts, not cures. Ignoring dental pain in favor of managing tension alone is like mopping the floor while leaving the faucet running—ineffective and counterproductive.
The takeaway? Tooth pain and headaches often intertwine through the pathway of muscle tension. Recognizing this connection allows for targeted intervention. For instance, a night guard prescribed by a dentist can prevent bruxism-induced tension, while regular dental check-ups catch issues before they escalate. By treating both the dental source and its muscular consequences, individuals can disrupt the cycle, finding relief not just in their mouth, but across their entire head and neck.
Frequently asked questions
Yes, a sore tooth can lead to a headache. Tooth pain, especially from issues like cavities, abscesses, or gum disease, can radiate to the head, causing referred pain or tension headaches.
A sore tooth can trigger headaches through shared nerve pathways. The trigeminal nerve, which supplies sensation to the face and mouth, also connects to the head. Inflammation or infection in the tooth can irritate this nerve, leading to head pain.
If you suspect your headache is linked to a sore tooth, consult a dentist to address the underlying dental issue. Over-the-counter pain relievers may provide temporary relief, but professional treatment is necessary to resolve the root cause.














