When it comes to extracting wisdom teeth, the type of dentist typically involved is an oral surgeon or a general dentist with experience in surgical procedures. Oral surgeons, also known as oral and maxillofacial surgeons, specialize in surgeries of the mouth, jaw, and face, making them highly qualified for complex wisdom tooth extractions. However, many general dentists also perform routine wisdom tooth removals, especially if the teeth are fully erupted and positioned correctly. In cases where the wisdom teeth are impacted or require more intricate removal, a referral to an oral surgeon is often recommended to ensure the procedure is handled safely and effectively.
| Characteristics | Values |
|---|---|
| Specialty | Oral and Maxillofacial Surgeon (OMS) or General Dentist (in simple cases) |
| Training | OMS: 4-6 years of surgical residency after dental school |
| Procedure Complexity | Handles complex extractions, impacted teeth, and surgical cases |
| Anesthesia Options | Local anesthesia, IV sedation, or general anesthesia |
| Facility | Often performed in a surgical center or hospital setting |
| Recovery Management | Provides post-operative care and manages complications |
| Cost | Higher due to specialized training and surgical expertise |
| Referral Needed | General dentists often refer to OMS for difficult cases |
| Scope of Practice | Focuses on surgeries involving the mouth, teeth, jaws, and face |
| Common Tools | Surgical instruments, imaging (X-rays, CT scans) |
| Patient Cases | Impacted wisdom teeth, infections, or teeth requiring surgical removal |
What You'll Learn

Oral Surgeon Expertise
Wisdom tooth extraction is a procedure that demands precision, skill, and a deep understanding of oral anatomy. Among dental professionals, oral surgeons stand out as the specialists uniquely qualified to handle complex cases. Their expertise extends beyond routine dentistry, encompassing advanced surgical techniques and a nuanced approach to patient care.
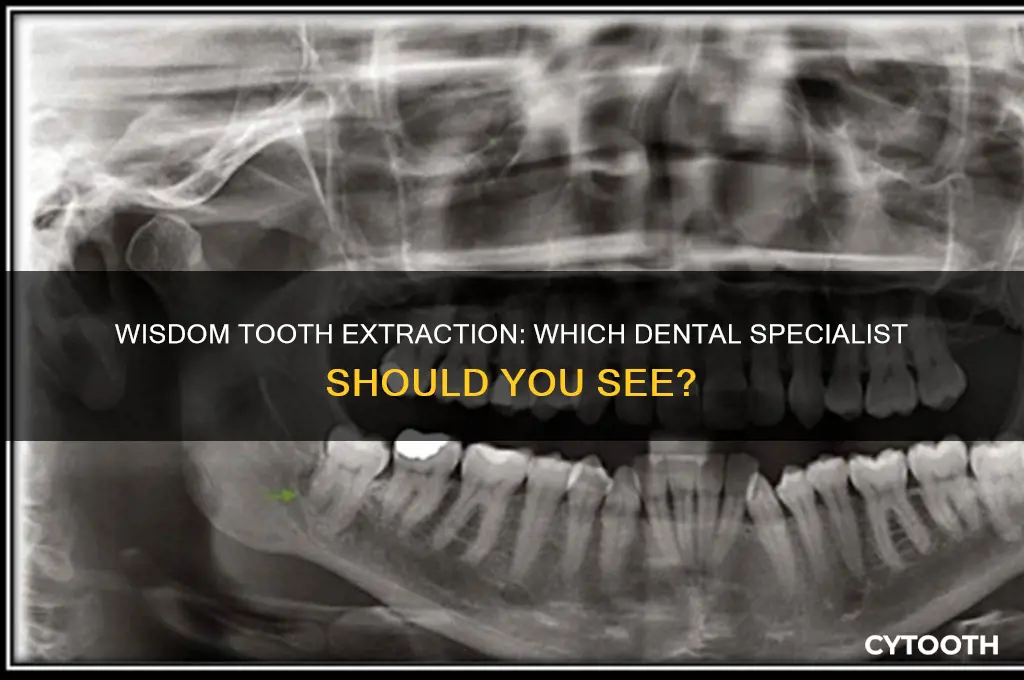
Consider the anatomical challenges of wisdom teeth: often impacted, angled, or partially erupted, these molars can complicate even straightforward extractions. Oral surgeons undergo an additional 4–6 years of training focused on surgical procedures, including anesthesia administration, soft tissue management, and bone manipulation. This specialized education equips them to address complications like nerve proximity, infection risk, or structural damage to adjacent teeth. For instance, in cases where a wisdom tooth lies close to the inferior alveolar nerve, an oral surgeon might employ 3D imaging to map the area, reducing the risk of permanent numbness—a complication that general dentists, lacking this advanced training, are less prepared to mitigate.
The procedural approach of an oral surgeon also differs significantly. While a general dentist might handle simple extractions, surgeons are trained to perform techniques like bone removal (osteotomy) or tooth sectioning, dividing the tooth into smaller pieces for safer extraction. Postoperative care is another area where their expertise shines. Surgeons often prescribe specific protocols, such as administering 400–800 mg of ibuprofen every 6–8 hours for pain management, paired with cold compresses for the first 24–48 hours to minimize swelling. They also monitor for dry socket (alveolar osteitis), a complication occurring in up to 5% of cases, and provide interventions like medicated dressings when necessary.
From a comparative standpoint, while some general dentists or orthodontists may perform wisdom tooth extractions, oral surgeons offer a higher threshold of safety and efficacy, particularly for high-risk patients—those with medical conditions like diabetes, bleeding disorders, or compromised immune systems. Their ability to administer intravenous sedation or general anesthesia in-office further distinguishes them, ensuring patient comfort during procedures that might otherwise be intolerable. For example, a patient with severe dental anxiety might receive a tailored sedation plan, such as a combination of midazolam (3–5 mg) and fentanyl (25–50 mcg) intravenously, allowing the surgeon to work efficiently while the patient remains relaxed.
In practice, knowing when to consult an oral surgeon can prevent complications. If a wisdom tooth is symptomatic (pain, swelling, infection), impacted, or disrupting orthodontic work, referral to a surgeon is advisable. Patients aged 18–25, the demographic most commonly requiring extractions, should seek a surgeon if their dentist expresses concern about the tooth’s position or accessibility. Ultimately, while not every wisdom tooth extraction requires an oral surgeon, their expertise is indispensable for cases that demand a higher level of technical proficiency and risk management.
Understanding Wisdom Teeth: Location, Purpose, and Common Concerns
You may want to see also

General Dentist Capabilities
General dentists are often the first point of contact for patients experiencing wisdom tooth discomfort. These practitioners are trained to perform routine extractions, including wisdom teeth removal, provided the teeth are fully erupted and positioned favorably. A 2020 survey by the American Dental Association revealed that 60% of general dentists regularly extract wisdom teeth in their practice, making them a common and accessible option for this procedure. However, their capability hinges on the complexity of the case. For instance, a wisdom tooth that has fully emerged into the correct position may require only a local anesthetic and a straightforward extraction, a task well within a general dentist’s skill set.
When considering a general dentist for wisdom tooth removal, patients should assess the tooth’s condition through a panoramic X-ray, which provides a comprehensive view of the jaw and tooth alignment. If the tooth is impacted (trapped beneath gum tissue or bone) or positioned at an awkward angle, the extraction may exceed a general dentist’s expertise. In such cases, they may refer the patient to an oral surgeon or periodontist. For example, a mesial impaction—where the tooth angles toward the front of the mouth—often requires specialized tools and techniques that general dentists may not routinely employ.
Despite limitations, general dentists offer several advantages for wisdom tooth removal. They are typically more accessible, with shorter wait times and lower costs compared to specialists. A 2021 study in the *Journal of Oral and Maxillofacial Surgery* found that straightforward wisdom tooth extractions performed by general dentists had success rates comparable to those of oral surgeons, with post-operative complications occurring in less than 5% of cases. Patients with fully erupted or minimally impacted wisdom teeth can often achieve satisfactory results without the need for a specialist, saving both time and money.
To determine if a general dentist is suitable for your wisdom tooth extraction, follow these steps: First, schedule a consultation to discuss symptoms and undergo an X-ray evaluation. Second, ask the dentist about their experience with similar cases and inquire about potential risks. Third, consider factors like anesthesia options—general dentists typically use local anesthesia, while oral surgeons may offer sedation for complex cases. Finally, weigh the convenience and cost against the complexity of the extraction. For uncomplicated cases, a general dentist is often the practical choice, but always prioritize safety and long-term oral health.
Pre-Wisdom Tooth Surgery Checklist: Essential Steps for a Smooth Recovery
You may want to see also

When Extraction is Necessary
Wisdom tooth extraction isn't always a rite of passage. While some people sail through life with these third molars causing no trouble, others face a barrage of problems that make removal a necessity.
Understanding when extraction is truly needed can save you from unnecessary pain, infection, and potential long-term dental issues.
Impaction: The Silent Threat
The most common reason for wisdom tooth extraction is impaction. This occurs when a tooth doesn't fully erupt through the gum line, often due to lack of space in the jaw. Impacted wisdom teeth can be angled incorrectly, pushing against neighboring teeth or even growing horizontally within the jawbone. This can lead to pain, swelling, and damage to adjacent teeth. In severe cases, impacted wisdom teeth can form cysts or tumors, requiring more complex surgical intervention.
If you experience persistent pain, swelling, or difficulty opening your mouth, consult a dentist immediately. Early detection of impaction can prevent further complications.
Crowding and Misalignment: A Recipe for Disaster
Even if wisdom teeth erupt fully, they can wreak havoc on your existing dental alignment. Our jaws are often not large enough to accommodate these late arrivals, leading to crowding and shifting of previously straightened teeth. This can undo years of orthodontic work and result in bite problems, difficulty chewing, and increased risk of tooth decay and gum disease.
Infection and Decay: A Breeding Ground for Trouble
Partially erupted wisdom teeth create a haven for bacteria. Food particles and debris can easily become trapped in the gum tissue surrounding these teeth, leading to infection (pericoronitis) and tooth decay. Symptoms include pain, swelling, bad breath, and difficulty swallowing. Left untreated, these infections can spread to other parts of the mouth and even the jawbone.
Preventive Measures: A Stitch in Time
While not all wisdom teeth require extraction, proactive monitoring is crucial. Regular dental checkups and X-rays allow your dentist to assess the position and development of your wisdom teeth. In some cases, early removal may be recommended to prevent future problems, especially if there's a family history of impacted wisdom teeth or jaw size limitations.
Remember, wisdom tooth extraction is a common procedure performed by oral surgeons or experienced general dentists. Don't ignore persistent pain or discomfort – early intervention can save you from a world of dental woes.
Cavity in Wisdom Tooth? Here’s What to Do Next
You may want to see also

Recovery and Aftercare Tips
Wisdom tooth extraction is typically performed by an oral surgeon or a general dentist with specialized training in surgical procedures. After the procedure, proper recovery and aftercare are crucial to prevent complications and ensure a smooth healing process. Here’s a focused guide to help you navigate the post-extraction phase effectively.
Immediate Post-Extraction Care: The First 24 Hours
The first day after surgery is critical for setting the stage for healing. Follow your dentist’s instructions meticulously. Apply an ice pack to the affected area in 20-minute intervals to reduce swelling. Avoid rinsing your mouth vigorously, spitting forcefully, or using straws, as these actions can dislodge the blood clot forming in the socket, leading to a painful condition called dry socket. Stick to soft, cool foods like yogurt, mashed potatoes, or smoothies, and avoid hot, spicy, or crunchy items that could irritate the surgical site. Take prescribed pain medications as directed—for example, ibuprofen (600 mg every 6 hours) or acetaminophen (500–1,000 mg every 4–6 hours) for pain management, but always follow your dentist’s dosage recommendations.
Managing Pain and Swelling: Days 2–7
Swelling and discomfort typically peak within the first 48 hours and gradually subside. Continue using cold compresses for the first 48 hours, then switch to warm compresses to promote circulation and healing. If swelling persists or worsens after 48 hours, contact your dentist. Over-the-counter pain relievers can be used as needed, but avoid aspirin, as it can increase bleeding. Elevate your head while sleeping to minimize swelling, and gently rinse your mouth with warm salt water (1/2 teaspoon of salt in 8 ounces of water) after meals to keep the area clean. Avoid smoking or vaping, as these can delay healing and increase infection risk.
Preventing Infection and Dry Socket: Week 1 and Beyond
Infection and dry socket are the most common complications after wisdom tooth extraction. To prevent them, maintain excellent oral hygiene, but be gentle around the surgical site. Brush your teeth carefully, avoiding the extraction area, and start using a saltwater rinse 24 hours after surgery. Avoid touching the wound with your fingers or tongue. If you notice signs of infection, such as fever, persistent pain, or foul-smelling discharge, seek immediate dental care. Dry socket typically occurs 3–5 days post-extraction and is characterized by severe pain and a visible empty socket. If suspected, your dentist may pack the site with a medicated dressing to promote healing.
Returning to Normal Activities: Timing and Precautions
Most people can resume light activities within 24–48 hours, but strenuous exercise or heavy lifting should be avoided for at least a week to prevent increased bleeding or swelling. Return to work or school when you feel comfortable, but listen to your body and rest as needed. Avoid alcohol for at least 48 hours, especially if taking prescription pain medications. Gradually reintroduce solid foods as tolerated, but continue to avoid hard, chewy, or sharp foods that could disrupt the healing site. Full recovery typically takes 1–2 weeks, but complete healing of the jawbone can take several months.
By following these recovery and aftercare tips, you can minimize discomfort, prevent complications, and ensure a successful healing process after wisdom tooth extraction. Always communicate with your dentist if you have concerns or experience unusual symptoms.
Identifying the Tooth Located Just in Front of Your Wisdom Tooth
You may want to see also

Cost and Insurance Coverage
The cost of wisdom tooth extraction can vary widely, typically ranging from $75 to $250 per tooth for simple extractions and $225 to $600 per tooth for surgical extractions. These figures are influenced by factors such as the complexity of the procedure, the dentist’s expertise, and geographic location. For instance, urban areas often have higher costs due to increased overhead expenses. Understanding these price ranges is the first step in budgeting for the procedure, but it’s equally important to explore how insurance coverage can offset these expenses.
Insurance coverage for wisdom tooth extraction depends on whether the procedure is deemed medically necessary. Most dental insurance plans cover a portion of the cost if the extraction is justified by issues like impaction, infection, or crowding. However, cosmetic or elective removals may not be covered. For example, a patient with a fully erupted, pain-free wisdom tooth might not receive insurance benefits. To maximize coverage, verify your plan’s specifics, including waiting periods, annual maximums, and whether oral surgeons or general dentists are in-network. Pro tip: Obtain pre-authorization from your insurer to avoid unexpected out-of-pocket costs.
For those without insurance, cost-saving strategies can make the procedure more affordable. Many dental offices offer payment plans or financing options, such as CareCredit, which allows patients to pay over time with little to no interest. Additionally, dental schools and community health clinics often provide extractions at reduced rates, performed by supervised students or resident dentists. While these options may require more research and flexibility, they can significantly lower expenses. For instance, a surgical extraction at a dental school might cost 30–50% less than at a private practice.
Comparing costs between general dentists and oral surgeons reveals another layer of financial consideration. General dentists typically charge less for simple extractions, but complex cases requiring surgical intervention are often referred to oral surgeons, whose fees are higher due to specialized training and equipment. Insurance may cover both providers, but reimbursement rates can differ. For example, an insurer might cover 80% of a general dentist’s fee but only 50% of an oral surgeon’s. Weighing the necessity of a specialist against potential costs is crucial for informed decision-making.
Finally, preventive measures can indirectly reduce long-term costs associated with wisdom tooth extraction. Regular dental check-ups, especially in the late teens and early twenties, allow for early detection of potential issues. Addressing problems like impaction or decay before they worsen can simplify the extraction process, reducing both the procedure’s complexity and cost. For instance, removing a mildly impacted tooth might cost $300, while waiting until it causes infection could escalate the price to $800 or more. Investing in preventive care is a practical way to manage expenses proactively.
Wisdom Tooth Removal: Understanding Anesthesia Types and Options
You may want to see also
Frequently asked questions
Oral surgeons and general dentists trained in surgical extractions typically perform wisdom tooth removals.
A regular dentist can extract wisdom teeth if the case is straightforward, but complex cases may require an oral surgeon.
An oral surgeon specializes in complex extractions and surgical procedures, while a general dentist handles routine dental care and simpler extractions.
No, orthodontists focus on teeth alignment and braces. Wisdom tooth extractions are handled by general dentists or oral surgeons.
See an oral surgeon if the wisdom teeth are impacted, deeply rooted, or if the extraction is expected to be complicated.













