The question of whether inner ear bones can break during a tooth extraction is a concern that arises due to the proximity of the oral cavity to the delicate structures of the ear. While tooth extractions are generally safe procedures, complications can occur, and the potential impact on nearby anatomical structures, such as the inner ear bones (ossicles), is a valid consideration. Although rare, there have been reported cases of temporal bone fractures or injuries to the middle and inner ear following dental procedures, including tooth extractions, particularly in complex or traumatic cases. Understanding the risks and taking preventive measures is essential for both dental professionals and patients to ensure a safe and complication-free experience.
| Characteristics | Values |
|---|---|
| Possibility of Inner Ear Bone Fracture | Extremely rare |
| Anatomical Proximity | Inner ear bones (ossicles) are located in the temporal bone, distant from the oral cavity and tooth extraction sites |
| Force Required for Fracture | Significant trauma or direct impact to the temporal bone, not typically generated during tooth extraction |
| Reported Cases | No documented cases of inner ear bone fracture due to tooth extraction |
| Risk Factors | None specific to tooth extraction; general risks include anatomical variations or pre-existing temporal bone conditions |
| Symptoms if Fracture Occurs | Hearing loss, dizziness, tinnitus, or ear pain (though these are highly unlikely in this context) |
| Diagnostic Methods | CT scan or MRI to assess temporal bone integrity (not routinely needed for tooth extraction) |
| Prevention | Standard tooth extraction protocols minimize risk; no specific precautions needed for inner ear bones |
| Conclusion | Inner ear bones breaking during tooth extraction is virtually impossible due to anatomical separation and lack of force transmission |
What You'll Learn

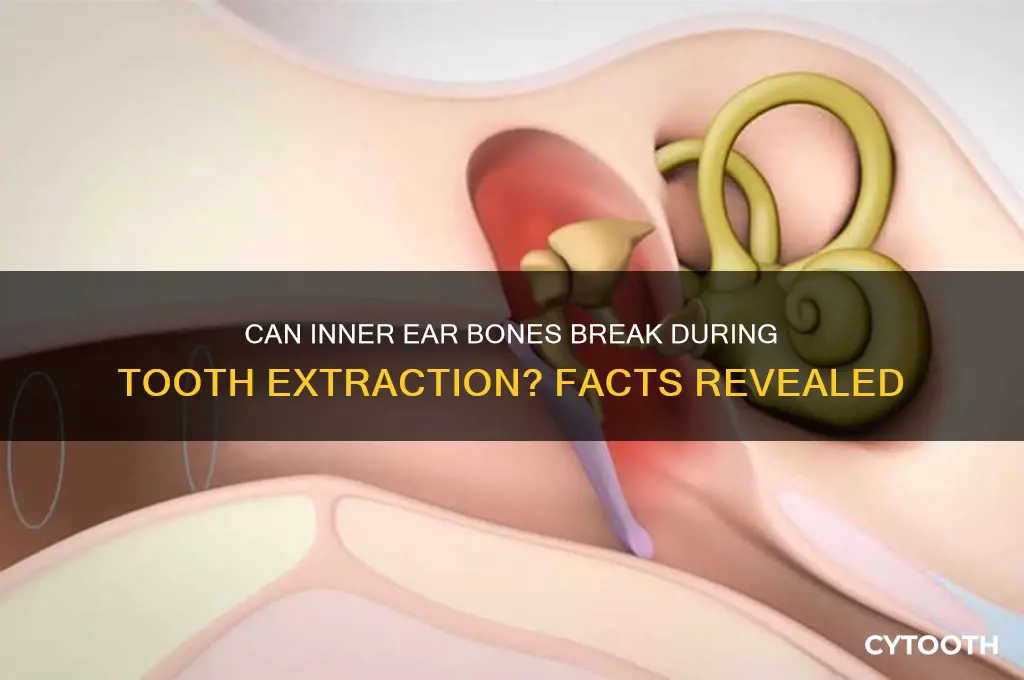
Anatomical Proximity of Inner Ear to Extraction Site
The inner ear bones, or ossicles, are among the smallest bones in the human body, nestled deep within the temporal bone of the skull. Their proximity to the oral cavity, particularly during dental procedures like tooth extractions, raises concerns about potential damage. Anatomically, the inner ear is separated from the extraction site by several layers of tissue, including the jawbone, muscles, and the tympanic membrane. However, the temporal bone, which houses the inner ear, is contiguous with the upper jaw (maxilla), meaning that excessive force or misdirected instruments could theoretically impact adjacent structures. Understanding this spatial relationship is crucial for both patients and practitioners to assess risks accurately.
Consider the maxillary molars, which are closest to the temporal bone and, by extension, the inner ear. During extraction, the use of elevators or forceps requires precision to avoid applying pressure to the surrounding bone. While the inner ear ossicles themselves are deeply protected, trauma to the temporal bone could lead to complications such as hearing loss or vertigo. For instance, a study in the *Journal of Oral and Maxillofacial Surgery* highlights cases where improper extraction techniques resulted in temporal bone fractures, though inner ear damage was rare. This underscores the importance of anatomical awareness during procedures in the posterior maxilla.
To minimize risk, dentists follow specific protocols when extracting teeth near the temporal bone. For upper molars, a buccal approach with controlled force is preferred, avoiding excessive lingual or lateral pressure. Radiographic imaging, such as panoramic X-rays or CT scans, is often used pre-operatively to assess the tooth’s root structure and its proximity to critical areas. Patients with anatomical variations, such as thin alveolar bone or pneumatized maxillary sinuses, may require additional precautions. Post-operative monitoring for symptoms like ear pain, tinnitus, or dizziness is essential, as these could indicate complications.
Comparatively, lower jaw (mandibular) extractions pose less risk to the inner ear due to the greater distance and the protective barrier of the skull base. However, the principle of anatomical awareness remains vital. For example, wisdom tooth extractions in the mandible can occasionally lead to inferior alveolar nerve damage, a reminder that even distant procedures require precision. In contrast, maxillary procedures demand a heightened focus on the vertical axis, given the inner ear’s vertical alignment with the upper jaw.
In conclusion, while the inner ear bones are well-protected by their anatomical location, their proximity to the maxillary extraction site necessitates careful technique and vigilance. Dentists must balance force application with spatial awareness, particularly for posterior maxillary teeth. Patients, meanwhile, should communicate any pre-existing conditions, such as temporal bone fractures or hearing issues, to ensure tailored care. By respecting the delicate interplay between oral and otic structures, practitioners can mitigate risks and ensure safe outcomes.
Infected Tooth Extraction: Link to Swollen Tonsils Explained
You may want to see also

Force Transmission During Dental Procedures
Dental procedures, particularly tooth extractions, involve the application of significant force in a highly sensitive area of the body. The maxilla and mandible, housing the teeth, are in close proximity to the temporal bones, which contain the delicate structures of the inner ear. This anatomical relationship raises concerns about force transmission and its potential impact on the ossicles—the three smallest bones in the body, crucial for hearing. Understanding the mechanics of force during dental interventions is essential to addressing the question of whether inner ear bones can be compromised.
The Force Dynamics in Tooth Extraction:
Imagine a scenario where a dentist applies force to extract a molar, a common procedure. The forceps grip the tooth, and with a controlled twist and pull, the tooth is removed. This action generates a force vector that travels through the jawbone. The key concern is the direction and magnitude of this force. If the force is misdirected or excessive, it could theoretically transmit through the temporal bone, potentially affecting the inner ear structures. However, the human skull's design includes natural shock-absorbing mechanisms, such as the periodontal ligament and the flexible joint of the mandible, which dissipate much of the force, reducing the risk to the inner ear.
A Comparative Perspective:
Consider the force required to fracture a bone. The ossicles, being the smallest bones, are indeed fragile, but their location within the protective confines of the middle ear provides a significant advantage. In contrast, the jawbone, a robust structure, can withstand considerable force. For instance, the average force required to extract a molar ranges from 50 to 200 Newtons, depending on various factors. This force is distributed across the tooth's roots and the surrounding bone, making it highly unlikely to cause a direct fracture of the inner ear bones. A study comparing the force transmission during dental procedures with the threshold for temporal bone fractures could provide valuable insights, potentially reassuring patients and practitioners alike.
Practical Considerations and Patient Safety:
Dental professionals employ techniques to minimize the risk of complications. For instance, using local anesthesia with vasoconstrictors can reduce bleeding and provide better visibility, allowing for more precise force application. Additionally, the use of surgical guides and advanced imaging techniques ensures accurate tooth extraction, reducing the likelihood of excessive force. Patients with specific concerns, such as those with a history of temporal bone fractures or inner ear disorders, should communicate these to their dentist. In such cases, a specialized approach might be warranted, possibly involving an otolaryngologist to ensure comprehensive care.
In summary, while the inner ear bones are delicate, the body's natural anatomy and the controlled techniques employed in dentistry make it highly improbable for these bones to break during a routine tooth extraction. However, understanding force transmission is crucial for dental professionals to refine their practices and address patient concerns effectively. This knowledge ensures that dental procedures remain safe and that patients can trust in the precision and care of modern dentistry.
Immediate Dental Implants: Can You Replace Extracted Teeth Right Away?
You may want to see also

Risk Factors for Inner Ear Damage
Inner ear damage during tooth extraction, though rare, is a serious concern that can lead to hearing loss, vertigo, or tinnitus. Understanding the risk factors is crucial for both patients and dental professionals to mitigate potential complications. Proximity of the extraction site to the inner ear structures, such as in wisdom tooth removal, increases the likelihood of trauma. The temporal bone, which houses the inner ear, is anatomically close to the molars, making this area particularly vulnerable during surgical procedures.
Anatomical variations play a significant role in elevating risk. Patients with smaller mandibular canals or those with abnormal positioning of the inferior alveolar nerve are more susceptible to inner ear damage. Additionally, pre-existing conditions like osteoporosis weaken bone density, making the temporal bone more fragile and prone to fractures during extraction. Age is another critical factor; older adults often experience bone demineralization, which can exacerbate the risk of inner ear injury.
The technique and force applied during extraction are equally important. Excessive pressure or improper use of dental instruments, such as elevators or forceps, can transmit trauma to the inner ear. For instance, a study published in the *Journal of Oral and Maxillofacial Surgery* highlighted that high-impact forces during third molar extractions were associated with a higher incidence of inner ear complications. Dentists must exercise caution, particularly when removing impacted teeth, to minimize the risk of damaging adjacent structures.
Certain medical conditions and medications can further amplify the risk. Patients with coagulation disorders or those taking anticoagulants, such as warfarin or aspirin, may experience prolonged bleeding, increasing the likelihood of inner ear trauma. Similarly, individuals with a history of otologic issues, such as chronic ear infections or Meniere’s disease, are more vulnerable to complications. A thorough medical history review is essential to identify these risk factors preoperatively.
Prevention strategies are key to avoiding inner ear damage. Dentists should employ gentle techniques, use appropriate sedation or anesthesia to reduce patient movement, and consider imaging studies like panoramic radiographs or CT scans to assess anatomical risks. Patients, especially those with identified risk factors, should discuss concerns with their dentist and explore alternative treatment options if necessary. Awareness and proactive measures can significantly reduce the incidence of this rare but debilitating complication.
Post-Extraction Infections: Causes, Symptoms, and Prevention Tips Explained
You may want to see also

Symptoms of Potential Inner Ear Injury
Inner ear injuries, though rare, can occur during dental procedures like tooth extractions due to proximity to the temporal bone and associated structures. Recognizing symptoms early is crucial for prompt intervention. One of the first indicators is sudden hearing loss or changes in one ear, which may present as muffled sounds, tinnitus (ringing), or difficulty understanding speech. This symptom often manifests immediately post-procedure or within hours, requiring urgent medical attention to prevent permanent damage.
Another critical symptom is vertigo or severe dizziness, often accompanied by nausea and imbalance. The inner ear’s vestibular system, responsible for balance, can be disrupted by trauma or inflammation. Patients may describe a spinning sensation or difficulty standing, even when the room is stationary. If these symptoms persist beyond 24 hours or worsen, an otolaryngologist should evaluate for potential damage to the semicircular canals or cochlea.
Facial numbness or weakness on the affected side is a red flag, suggesting injury to the facial nerve (cranial nerve VII), which runs near the inner ear. This may appear as drooping of the eyelid, difficulty closing the eye, or asymmetry when smiling. While this symptom is less common, it demands immediate attention to rule out complications like temporal bone fractures or nerve compression.
Lastly, ear pain or discharge localized to the affected side should not be overlooked. Blood or clear fluid draining from the ear post-extraction indicates a possible perforation or fracture of the temporal bone. Patients should avoid blowing their nose or straining, as increased pressure can exacerbate the injury. Applying a sterile dressing and seeking emergency care is essential to prevent infection or further damage.
In summary, symptoms like unilateral hearing loss, vertigo, facial weakness, and ear discharge warrant immediate evaluation after a tooth extraction. Early diagnosis and management, often involving imaging (CT/MRI) and specialist consultation, can mitigate long-term consequences. Patients should monitor for these signs closely and communicate any concerns to their healthcare provider promptly.
Can an Infected Tooth Be Extracted? Risks, Benefits, and Recovery Explained
You may want to see also

Preventive Measures and Surgical Techniques
The proximity of the inner ear to the oral cavity during dental procedures necessitates meticulous planning and execution to avoid complications. Preventive measures begin with a comprehensive pre-operative assessment, including detailed imaging studies such as cone-beam computed tomography (CBCT). This allows surgeons to visualize the spatial relationship between the tooth roots, mandibular canal, and adjacent structures, reducing the risk of inadvertent damage to the inner ear bones, which are separated by only millimeters in some cases.
Surgical techniques play a pivotal role in minimizing trauma to the temporomandibular joint and surrounding structures. For instance, the use of piezoelectric instruments offers precision cutting with reduced vibration compared to traditional rotary tools, thereby decreasing the likelihood of microfractures in the temporal bone. Additionally, slow and controlled extraction methods, coupled with copious irrigation to prevent heat buildup, are essential. In cases involving lower molars, sectioning the tooth into smaller fragments can mitigate excessive force application, a common cause of iatrogenic fractures.
Postoperative care is equally critical in preventing complications. Patients should be advised to avoid strenuous activities, such as heavy lifting or vigorous nose blowing, for at least 72 hours post-extraction. Anti-inflammatory medications like ibuprofen (400–600 mg every 6 hours) can help manage swelling and pain, but should be used cautiously in patients with renal or gastrointestinal issues. Cold compresses applied for 20 minutes on, 20 minutes off, during the first 48 hours can reduce edema and hematoma formation, indirectly protecting the delicate structures of the inner ear.
Comparatively, alternative procedures like guided tissue regeneration or implant placement require even greater precision due to their invasive nature. Surgeons must adhere to strict protocols, such as maintaining a safe distance of at least 2 mm from the inferior alveolar nerve and avoiding excessive pressure on the lingual plate. Patient education is paramount; individuals with pre-existing conditions like osteoporosis or those on anticoagulants (e.g., warfarin, aspirin) may face heightened risks and should be managed collaboratively with their primary care provider to adjust medication regimens prior to surgery.
In conclusion, while the direct fracture of inner ear bones during tooth extraction is rare, its prevention hinges on a multidisciplinary approach combining advanced imaging, refined surgical techniques, and vigilant postoperative care. By adhering to these measures, practitioners can significantly reduce the incidence of complications, ensuring safer outcomes for patients undergoing dental procedures.
Can Infections Lead to Bleeding After Tooth Extraction? Find Out Here
You may want to see also
Frequently asked questions
No, the inner ear bones (ossicles) are located deep within the temporal bone of the skull and are not anatomically connected to the teeth or jaw. A tooth extraction cannot cause them to break.
While extremely rare, damage to the inner ear is possible if there is an infection or anatomical abnormality near the extraction site. However, this is not related to the inner ear bones breaking.
No, tooth extraction cannot cause hearing loss by damaging the inner ear bones. Hearing loss after extraction, if it occurs, is typically due to nerve damage, infection, or other complications unrelated to the inner ear bones.
No, the inner ear bones are located in the temporal bone, far from the teeth and jaw. They are not in proximity to the extraction site and cannot be affected by the procedure.
If you experience ear pain or hearing issues after a tooth extraction, consult your dentist or an ENT specialist immediately. These symptoms may be unrelated to the extraction and could indicate an infection, nerve issue, or other condition.