After a molar tooth extraction, the gums in the affected area typically appear swollen, red, and may have a small blood clot forming in the socket, which is a normal part of the healing process. The gum tissue around the extraction site might look slightly bruised or discolored due to minor bleeding and inflammation. Initially, the socket will be an empty space, but over time, the gums will begin to close in as new tissue forms. It’s important to follow post-extraction care instructions to prevent complications like dry socket, which can cause the gums to appear pale or gray and lead to severe pain. Proper healing will gradually restore the gums to a more natural appearance, though the area may remain slightly sensitive for a few weeks.
| Characteristics | Values |
|---|---|
| Appearance | Initially swollen, red, and possibly bruised |
| Color | Red or dark pink due to inflammation; may have small blood clots |
| Texture | Soft and tender to the touch; may feel rough due to sutures or healing tissue |
| Shape | Indentation or socket where the tooth was extracted; edges may appear irregular |
| Bleeding | Minimal oozing is normal for the first 24–48 hours; blood clots may be visible |
| Swelling | Mild to moderate swelling around the extraction site and surrounding gums |
| Healing Tissue | White or pale pink granulation tissue begins to form within a few days |
| Sutures | Stitches may be present, appearing as black, white, or clear threads |
| Pain/Sensitivity | Gums may be sensitive or painful, especially when touched or during healing |
| Timeframe | Initial changes visible immediately; full healing of gums takes 1–2 weeks |
| Infection Signs | If gums become excessively red, swollen, or pus is present, infection may be likely |
What You'll Learn

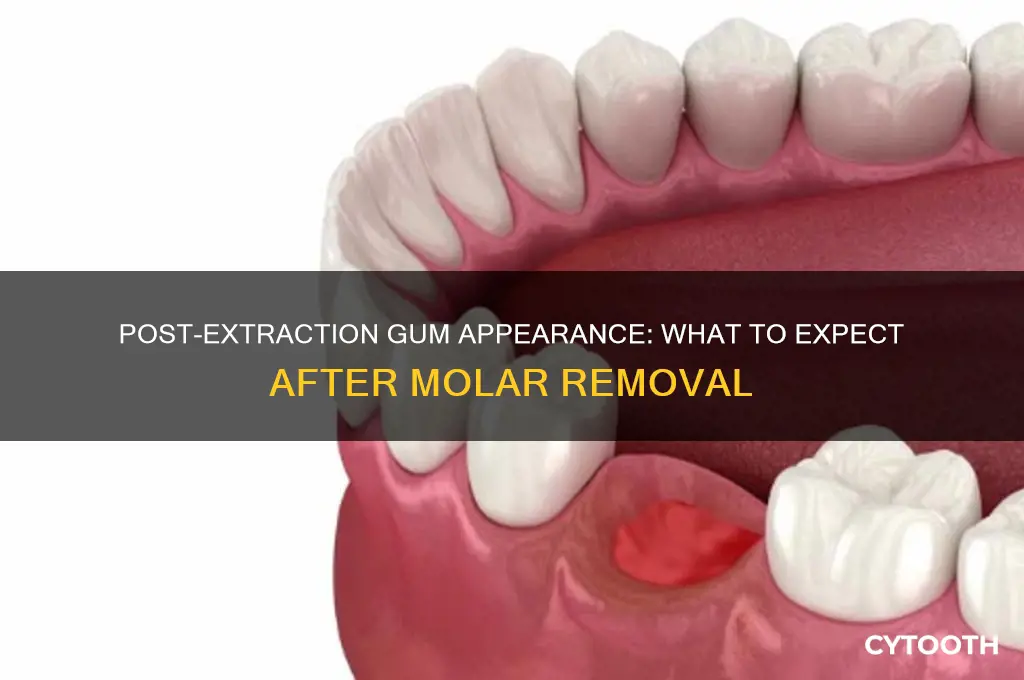
Immediate Post-Extraction Appearance
Immediately following a molar extraction, the gum tissue at the extraction site will appear noticeably altered, reflecting the body’s initial response to trauma. The socket itself is likely to be filled with a blood clot, which forms within the first 15–30 minutes post-extraction. This clot is essential for healing, appearing as a dark red or black mass depending on oxygen exposure. Surrounding gum tissue may be swollen, slightly bruised, or discolored due to localized inflammation and bleeding. It’s critical to avoid disturbing this clot, as dislodging it can lead to a painful condition called dry socket, delaying recovery by up to 10–14 days.
From a comparative perspective, the immediate post-extraction appearance of gums differs significantly from their pre-extraction state. Healthy gums typically exhibit a firm, pink texture with a stippled surface. Post-extraction, the area around the socket may appear smoother and darker due to the blood clot and initial swelling. In contrast to routine dental cleanings or fillings, where gums return to normal within hours, extraction sites take 24–48 hours for swelling to peak before gradually subsiding. Patients should expect this temporary distortion as a normal part of the healing process, not a cause for alarm.
For those managing post-extraction care, specific steps can minimize discomfort and promote healing. Apply a cold compress to the cheek for 15–20 minutes at a time during the first 24 hours to reduce swelling. Avoid vigorous rinsing, spitting, or using straws for the first 24 hours to protect the blood clot. After the first day, gently rinse with a warm saltwater solution (1/2 teaspoon of salt in 8 ounces of water) to keep the area clean. Over-the-counter pain relievers like ibuprofen (600 mg every 6 hours) or acetaminophen (1000 mg every 6 hours) can manage pain, but follow dosage instructions carefully.
A persuasive argument for adhering to post-extraction guidelines lies in the consequences of neglect. Failing to protect the blood clot increases the risk of dry socket, which occurs in 2–5% of cases but is largely preventable. Symptoms include severe pain radiating to the ear or neck, bad breath, and an empty socket visible in the mirror. Treatment involves dressing changes and pain management, significantly extending recovery time. By contrast, patients who follow care instructions typically experience minimal complications, with gum tissue beginning to close over the socket within 3–4 days and complete healing in 1–2 months.
Descriptively, the evolution of gum appearance in the days following extraction provides a roadmap for recovery. By day 3, swelling should noticeably decrease, and the blood clot may begin to lighten in color. Around day 7, granulation tissue—a pale pink, bumpy surface—starts to form as new blood vessels and connective tissue develop. By week 2, the socket is largely covered, though the gum contour may remain slightly uneven until bone remodeling completes over the next several months. Monitoring these changes ensures patients recognize normal healing versus potential complications, fostering confidence in the recovery process.
Understanding Dry Socket: Causes and Prevention After Tooth Extraction
You may want to see also

Normal Gum Healing Process
After a molar extraction, the gums undergo a transformative healing process, typically beginning with a blood clot forming in the socket within the first 24 hours. This clot is crucial as it acts as a protective barrier and foundation for new tissue growth. Initially, the area may appear dark red or white, depending on the clot’s stage and exposure to air or food particles. Avoid disturbing this clot by refraining from vigorous rinsing, spitting, or using straws for at least 24–48 hours, as dislodging it can lead to a painful condition called dry socket.
As healing progresses, the gum tissue around the extraction site begins to regenerate. Within 3–7 days, you may notice a pale pink or slightly swollen appearance as new granulation tissue forms. This tissue is rich in blood vessels and helps rebuild the gum structure. During this phase, mild discomfort or a tingling sensation is normal, but persistent pain or swelling warrants a call to your dentist. Keep the area clean by gently rinsing with warm salt water after meals to prevent infection and promote healing.
By the end of the first week, the gum tissue should start to firm up and blend more seamlessly with the surrounding gums. The extraction site may still appear slightly indented or uneven, but this is a natural part of the healing process. Avoid probing the area with your tongue or fingers, as this can introduce bacteria and delay recovery. If you notice any pus, foul odor, or worsening pain, these could be signs of infection and require immediate dental attention.
Around 2–3 weeks post-extraction, the gums should be closer to their pre-extraction appearance, though complete healing can take up to 6 months. The indentation in the gum line will gradually fill in as bone and tissue regenerate. To support this process, maintain good oral hygiene, avoid smoking or tobacco use, and follow a soft, nutrient-rich diet to provide essential vitamins and minerals for tissue repair. Patience is key, as rushing the healing process can lead to complications.
Post-Extraction Care: Essential Tips for Healing After a Tooth Extraction
You may want to see also

Signs of Infection or Complications
After a molar extraction, the gums typically appear swollen, slightly bruised, and may have a small blood clot at the extraction site. However, it’s crucial to monitor for signs of infection or complications, as these can escalate quickly if left untreated. One of the earliest indicators is persistent or worsening pain that doesn’t subside with over-the-counter pain relievers like ibuprofen (600–800 mg every 6–8 hours, as directed by a dentist). If pain intensifies after the first 48 hours, it may signal an infection or dry socket, a condition where the blood clot dislodges, exposing bone and nerves.
Another red flag is unusual discharge or odor from the extraction site. Healthy healing gums should not emit a foul smell or produce pus. If you notice greenish-yellow or grayish discharge, or if the area smells unpleasant, this could indicate a bacterial infection. Similarly, fever, chills, or swollen lymph nodes in the neck are systemic signs that the body is fighting an infection. These symptoms warrant immediate dental attention, as antibiotics (e.g., amoxicillin 500 mg three times daily, prescribed by a dentist) may be necessary to prevent further complications.
Visually, infected gums may appear unusually red, inflamed, or develop white or yellow patches near the extraction site. Compare the affected area to the surrounding gum tissue—healthy gums should gradually return to a pale pink color as they heal. If the redness spreads or the gums feel hot to the touch, this suggests infection. Additionally, prolonged bleeding (beyond 24 hours) or oozing that doesn’t stop with gentle pressure and a gauze pad could indicate a problem with clotting or infection.
Prevention is key to avoiding complications. Follow post-extraction care instructions meticulously: avoid smoking, using straws, or rinsing vigorously for the first 24 hours, as these actions can dislodge the blood clot. Rinse gently with warm salt water (1/2 teaspoon of salt in 8 ounces of water) starting 24 hours after the procedure to keep the area clean. If you notice any of the above signs, contact your dentist promptly—early intervention can prevent minor issues from becoming major problems.
Post-Tooth Extraction Beverages: Safe and Soothing Drink Options to Enjoy
You may want to see also

Gum Tissue Regeneration Timeline
After a molar extraction, the gum tissue begins a complex healing process that unfolds in distinct phases. The initial 24–48 hours post-extraction are marked by clot formation, a critical step to prevent dry socket and initiate healing. During this period, the gums appear swollen, red, and may have a slight blood tinge. Patients are advised to avoid rinsing vigorously, spitting forcefully, or using straws to protect the clot. Pain management with over-the-counter medications like ibuprofen (600–800 mg every 6–8 hours) or acetaminophen (500–1000 mg every 4–6 hours) is recommended, following the dentist’s guidelines.
By days 3–7, the clot matures into granulation tissue, a pinkish, bumpy area that signals the beginning of gum tissue regeneration. This phase is characterized by reduced swelling and pain, though the gums may still appear uneven or raw. Patients should continue gentle oral hygiene, using a soft-bristled toothbrush and avoiding the extraction site. Saltwater rinses (1/2 teaspoon of salt in 8 ounces of warm water) can aid healing, but chlorhexidine mouthwash should only be used if prescribed, as it can disrupt natural tissue repair in some cases.
Between weeks 2–4, the gums undergo significant transformation as fibroblasts and collagen fibers rebuild the tissue. The extraction site becomes less noticeable, with the gums appearing smoother and closer to their pre-extraction color. However, complete regeneration of the gum contour may take 3–6 months, depending on factors like age, overall health, and smoking habits. Patients over 50 or those with diabetes may experience slower healing, emphasizing the need for diligent aftercare.
Beyond the first month, the focus shifts to long-term tissue stability. Bone regeneration, which supports the gums, continues for 3–6 months, during which the gums may subtly shift in shape. To support this process, a diet rich in vitamin C (found in citrus fruits, bell peppers, and broccoli) and protein (lean meats, eggs, and legumes) is beneficial. Avoiding tobacco and limiting alcohol intake are critical, as both impair blood flow and delay healing. Regular follow-ups with the dentist ensure the gums are healing properly and address any complications early.
By month 6, the gums typically achieve their final appearance, though minor adjustments may continue for up to a year. The regenerated tissue may not perfectly match the original gum line, especially if bone loss occurred prior to extraction. For those seeking faster or more predictable results, advanced treatments like platelet-rich fibrin (PRF) or growth factor therapies can be discussed with a periodontist. These methods accelerate healing by concentrating the body’s natural regenerative cells at the extraction site, reducing recovery time by 20–30%.
Tools and Techniques Dentists Use for Tooth Extraction Explained
You may want to see also

Expected Color and Texture Changes
Immediately following a molar extraction, the gum tissue at the site will typically appear pale and swollen, a direct result of trauma and increased blood flow to the area. This initial paleness is often accompanied by a smooth, almost glossy texture due to the absence of the tooth and the body’s immediate response to seal the wound. Within the first 24–48 hours, expect a shift toward pinkish-red discoloration as inflammation peaks, signaling the body’s active healing process. This redness is normal and should gradually subside as the gum tissue begins to repair itself.
As healing progresses, the gum tissue will transition from a smooth, swollen surface to a rougher, granulated texture, particularly around days 3–7. This change indicates the formation of a blood clot and the early stages of tissue regeneration. The color will deepen to a darker pink or even purplish hue, which is a healthy sign of new blood vessel formation. Avoid disturbing this area—vigorous rinsing, spitting, or probing with your tongue can dislodge the clot, leading to a painful condition called dry socket.
By the second week, the gum tissue should begin to flatten and firm up, with the texture becoming less granular and more uniform. The color will lighten to a healthy pink, resembling the surrounding gum tissue. At this stage, the clot has matured into a protective fibrin mesh, and epithelial cells are actively closing the wound. Patients over 40 may notice slower healing due to reduced blood flow and collagen production, so maintaining a soft diet and avoiding smoking is critical to prevent complications.
Beyond the third week, the extraction site will blend seamlessly with the surrounding gums, both in color and texture. The tissue will feel smooth and stable, with no visible signs of redness or inflammation. However, if the area remains tender, swollen, or oozes pus after this period, seek immediate dental care, as it may indicate infection. To aid healing, rinse gently with a 50/50 saline solution (1/2 teaspoon salt per cup of warm water) twice daily, starting 24 hours post-extraction.
Post-Extraction Care: Common Medications Dentists Prescribe After Tooth Removal
You may want to see also
Frequently asked questions
Immediately after a molar tooth is pulled, the gums may appear swollen, red, and slightly bruised around the extraction site. A blood clot will typically form in the socket, which looks like a dark, gelatinous mass.
Gums usually begin to heal within a few days, with swelling and redness reducing gradually. Complete healing of the gums can take 1–2 weeks, though the socket may take 6–8 weeks to fully close.
Yes, it’s normal for gums to appear slightly pale or white immediately after extraction due to reduced blood flow or the presence of a blood clot. However, persistent paleness or signs of infection (e.g., pus, severe pain) should be evaluated by a dentist.














