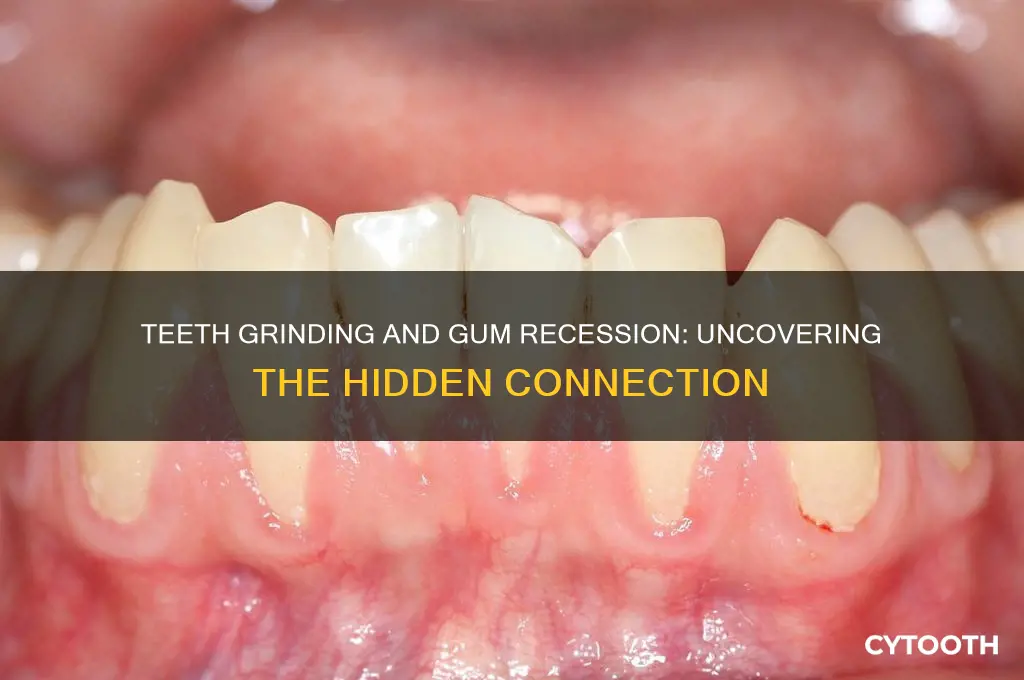
Teeth grinding, also known as bruxism, is a common habit that can have significant impacts on oral health, and one concern often raised is its potential link to gum recession. When individuals grind their teeth, especially during sleep, the excessive force exerted on the teeth and surrounding tissues can lead to inflammation and damage over time. This chronic pressure may contribute to the gradual wearing away of the gum tissue, causing it to recede and expose more of the tooth's root. As gum recession progresses, it can result in increased tooth sensitivity, a higher risk of cavities, and even tooth mobility. Understanding the relationship between bruxism and gum recession is essential for developing effective preventive measures and treatment strategies to maintain optimal oral health.
What You'll Learn
- Teeth Grinding Mechanics: How clenching and grinding exert excessive force on gums, potentially accelerating recession
- Gum Tissue Stress: Chronic pressure from bruxism weakens gum fibers, leading to detachment from teeth
- Inflammation Link: Bruxism increases gum inflammation, compromising blood flow and tissue health
- Tooth Mobility Effect: Grinding loosens teeth, exposing roots and causing gums to recede
- Preventive Measures: Mouthguards and stress management reduce grinding, minimizing gum recession risk

Teeth Grinding Mechanics: How clenching and grinding exert excessive force on gums, potentially accelerating recession
Teeth grinding, or bruxism, is a mechanical force multiplier. When you clench or grind, the pressure exerted on your teeth can reach up to 250 pounds per square inch—far exceeding the 10-20 pounds typical for chewing. This excessive force doesn’t just wear down enamel; it radiates through the periodontal ligament, the shock-absorbing tissue connecting teeth to bone, and transfers stress directly to the gums. Over time, this chronic strain weakens the gum tissue’s attachment to the tooth, making it more susceptible to recession. Think of it as overloading a rubber band until it stretches beyond recovery.
To visualize the impact, consider the gums as a protective collar around each tooth. During grinding, the repetitive, forceful contact between teeth creates micro-trauma in the gum fibers. This trauma disrupts blood flow and nutrient delivery to the tissue, hindering its ability to repair itself. For adults aged 30-50, who are most prone to bruxism, this process can accelerate gum recession by 2-3 times the normal rate, especially if grinding occurs nightly. Practical tip: monitor for signs like tooth sensitivity or gum line changes, and consider a night guard to redistribute the force.
The mechanics of grinding also involve a lateral component, where teeth slide against each other horizontally. This motion acts like a saw, gradually cutting into the gum line. Unlike vertical forces, which primarily stress the periodontal ligament, lateral forces directly abrade the gums. Studies show that individuals with severe bruxism experience recession at an average rate of 0.5 millimeters per year, compared to 0.1 millimeters in non-grinders. To mitigate this, dentists recommend limiting hard foods (e.g., ice or nuts) during the day, as they exacerbate the wear pattern.
A comparative analysis reveals that clenching and grinding differ in their effects. Clenching, a static action, compresses gums uniformly, while grinding’s dynamic motion creates uneven stress points. This distinction matters because uneven stress is more likely to cause localized recession, particularly in areas where teeth meet. For instance, the first molars, which bear the brunt of grinding, often show recession sooner than incisors. Addressing this requires a two-pronged approach: reducing the force (via stress management or Botox injections) and protecting the gums (with fluoride treatments or antimicrobial rinses).
Finally, the interplay between bruxism and gum health underscores the need for early intervention. A 2022 study found that 70% of untreated bruxism cases led to moderate gum recession within 5 years. For those over 40, whose gums are naturally thinning, this timeline shortens. Practical steps include tracking grinding episodes with a sleep app, using a humidifier to prevent dry mouth (a bruxism trigger), and scheduling biannual dental checkups to catch recession early. By understanding the mechanics, you can act before the force becomes irreversible damage.
Coronavirus and Oral Health: Exploring Its Impact on Teeth and Gums
You may want to see also

Gum Tissue Stress: Chronic pressure from bruxism weakens gum fibers, leading to detachment from teeth
Chronic teeth grinding, or bruxism, exerts relentless pressure on the periodontal ligaments and gum fibers that anchor teeth in place. Over time, this mechanical stress fatigues the collagen fibers within the gingival tissue, compromising their elasticity and resilience. Imagine a rubber band stretched repeatedly—it weakens, loses its shape, and eventually snaps. Similarly, gum fibers under constant strain from bruxism begin to fray and detach from the tooth surface, creating gaps where bacteria can infiltrate and exacerbate gum recession.
To mitigate this, consider a two-pronged approach: reducing bruxism and strengthening gum tissue. For bruxism management, a custom-fitted night guard, worn during sleep, redistributes occlusal forces evenly across the dental arch, minimizing localized pressure. Adults aged 18–65 with moderate to severe grinding may benefit from wearing a guard nightly, though compliance is key—effectiveness drops if usage falls below 5 nights per week. Pair this with stress-reduction techniques like progressive muscle relaxation or mindfulness, as bruxism often spikes during periods of heightened anxiety.
Simultaneously, focus on gum tissue fortification. Incorporate 1,000–1,200 mg of vitamin C daily (through diet or supplements) to support collagen synthesis, essential for gum fiber repair. Avoid aggressive brushing—use a soft-bristled toothbrush at a 45-degree angle with gentle, circular motions to prevent further trauma. For targeted care, apply a pea-sized amount of 0.12% chlorhexidine gel along the gumline twice weekly to reduce inflammation and bacterial load, but limit use to 2–4 weeks to avoid staining.
Comparatively, untreated bruxism accelerates recession at a rate 2.5 times faster than in non-grinders, according to a 2021 study in the *Journal of Periodontology*. Conversely, patients who combined night guard use with improved oral hygiene saw a 60% reduction in recession progression over 18 months. This highlights the importance of addressing both the cause (bruxism) and the effect (gum stress) for optimal outcomes.
Finally, monitor for early warning signs: tooth sensitivity, visible wear facets, or gums that appear thinner or redder than usual. If recession exceeds 2 mm in depth or exposes root surfaces, consult a periodontist for interventions like gum grafting. While bruxism’s impact on gums is insidious, proactive measures can halt its progression, preserving both tissue integrity and dental health.
Zyns and Oral Health: Debunking Myths About Teeth and Gums
You may want to see also

Inflammation Link: Bruxism increases gum inflammation, compromising blood flow and tissue health
Bruxism, or teeth grinding, isn’t just a noisy nighttime habit—it’s a silent saboteur of gum health. The constant pressure and friction from grinding create micro-traumas in the gum tissue, triggering an inflammatory response. This inflammation, while the body’s natural defense mechanism, becomes problematic when chronic. Over time, it disrupts blood flow to the gums, starving them of essential nutrients and oxygen. Without adequate circulation, gum tissue weakens, making it more susceptible to recession. Think of it as overworking a muscle without recovery; the tissue breaks down, unable to repair itself effectively.
To understand the severity, consider this analogy: inflammation in gums is like a slow-burning fire. Initially, it’s contained, but without intervention, it spreads, damaging surrounding structures. Bruxism fuels this fire by repeatedly stressing the gums, causing them to pull away from the teeth. Studies show that individuals with bruxism are 2.5 times more likely to experience gum recession compared to non-grinders. The inflammation also compromises the periodontal ligament, the tissue anchoring teeth to the jawbone, further destabilizing tooth structure and accelerating recession.
Practical steps can mitigate this risk. First, address the root cause: stress and misaligned teeth are common bruxism triggers. Stress management techniques like mindfulness or progressive muscle relaxation can reduce grinding episodes. For misalignment, orthodontic treatments or occlusal adjustments by a dentist may be necessary. Second, protect gums during sleep with a custom-fitted night guard, which acts as a cushion, absorbing the force of grinding. Finally, maintain impeccable oral hygiene to reduce inflammation. Use a soft-bristled toothbrush and non-alcoholic mouthwash, as alcohol can dry out gums, exacerbating inflammation.
A cautionary note: over-the-counter night guards may seem convenient, but they lack the precision of custom-fitted ones, potentially worsening bite issues. Similarly, ignoring bruxism under the assumption it’s harmless can lead to irreversible gum damage. Regular dental check-ups are crucial for early detection and intervention. For those over 40, who are more prone to gum recession due to age-related tissue thinning, monitoring bruxism becomes even more critical. Pairing professional care with at-home strategies creates a robust defense against inflammation-driven recession.
The takeaway is clear: bruxism’s inflammation link isn’t just theoretical—it’s a tangible threat to gum health. By understanding the mechanism and taking proactive measures, individuals can break the cycle of inflammation and protect their gums. It’s not about eliminating grinding overnight but about managing its impact effectively. With the right tools and awareness, preserving gum tissue becomes an achievable goal, ensuring a healthier smile for years to come.
Can Receding Gums Regrow? Debunking Myths and Exploring Solutions
You may want to see also

Tooth Mobility Effect: Grinding loosens teeth, exposing roots and causing gums to recede
Teeth grinding, or bruxism, exerts excessive force on the teeth and surrounding structures, leading to a phenomenon known as tooth mobility. This occurs when the periodontal ligaments—the fibers that anchor teeth to the jawbone—become damaged or inflamed. Over time, the constant pressure from grinding weakens these ligaments, causing teeth to shift or loosen. As teeth lose their stability, the gums begin to recede, exposing the sensitive roots. This exposure not only increases sensitivity to hot, cold, and sweet stimuli but also leaves the roots vulnerable to decay and infection.
Consider the mechanics: each grinding episode can generate forces up to 250 pounds per square inch, far exceeding the 15–20 pounds exerted during normal chewing. This repeated stress accelerates the breakdown of gum tissue and bone, hastening recession. For instance, a 35-year-old patient with untreated bruxism might notice their gums pulling away from their teeth within 3–5 years, compared to a non-grinder of the same age. Night guards, which distribute force evenly, can reduce this risk by up to 70%, according to dental studies.
To mitigate the tooth mobility effect, start by identifying triggers for grinding, such as stress or caffeine consumption after 3 PM. Incorporate stress-relief techniques like progressive muscle relaxation or mindfulness exercises for 10–15 minutes daily. If grinding occurs during sleep, consult a dentist for a custom-fitted night guard. Over-the-counter options are available, but they may not provide adequate protection for severe cases. Additionally, avoid hard or chewy foods that exacerbate pressure on loosened teeth, and use a soft-bristled toothbrush to minimize further gum irritation.
Comparatively, while gum recession can also result from poor oral hygiene or aggressive brushing, bruxism-induced recession is unique in its mechanical origin. Unlike plaque buildup, which attacks gums chemically, grinding physically displaces teeth, creating gaps where gums once adhered. This distinction highlights the need for targeted interventions, such as splint therapy or orthodontic adjustments, to stabilize teeth and prevent further recession. Early intervention is critical; once gum tissue is lost, it cannot regenerate, making prevention and prompt treatment essential.
Finally, monitor for warning signs like increased tooth wobbliness, heightened sensitivity, or visible root exposure. If detected, schedule a dental evaluation immediately. A dentist may recommend periodontal procedures like gum grafting to cover exposed roots or scaling and root planing to remove irritants causing inflammation. Combining these treatments with bruxism management can halt progression and preserve oral health. Remember, addressing tooth mobility not only protects gums but also safeguards the longevity of your teeth.
Teeth Clenching and Gum Recession: Uncovering the Hidden Connection
You may want to see also

Preventive Measures: Mouthguards and stress management reduce grinding, minimizing gum recession risk
Teeth grinding, or bruxism, exerts excessive force on the teeth and gums, accelerating tissue wear and contributing to gum recession. While not the sole cause, it significantly compounds risk factors like poor oral hygiene or misaligned bites. Preventive measures, however, can mitigate this damage effectively. Mouthguards, for instance, act as a physical barrier, redistributing grinding forces and protecting gum lines from direct trauma. Simultaneously, addressing the root cause—often stress—through techniques like mindfulness or cognitive behavioral therapy reduces the frequency and intensity of grinding episodes. Together, these strategies form a dual defense against the progression of gum recession.
Consider the mechanics: a custom-fitted night guard, typically made of soft acrylic or silicone, cushions the impact between upper and lower teeth during sleep, the prime time for unconscious grinding. Dentists recommend wearing these devices nightly, especially for individuals with moderate to severe bruxism. Over-the-counter options are available, but professional fittings ensure optimal protection and comfort. For children and adolescents, whose jaws are still developing, pediatric dentists may prescribe age-appropriate guards to prevent early-onset gum issues. Consistency is key—even minor nightly grinding, when unchecked, can lead to cumulative damage over years.
Stress management, on the other hand, tackles the behavioral triggers of bruxism. Adults aged 25–45, particularly those in high-pressure environments, benefit from incorporating relaxation techniques into their routines. Progressive muscle relaxation, for example, involves tensing and releasing facial muscles to reduce tension, a practice that can be done in 10-minute sessions before bed. Similarly, mindfulness meditation, practiced for 15–20 minutes daily, has been shown to lower stress hormones like cortisol, indirectly reducing grinding tendencies. For those with persistent stress, combining these techniques with professional counseling amplifies results, creating a holistic approach to oral and mental health.
Comparing these methods reveals their complementary strengths. Mouthguards provide immediate physical protection, ideal for managing existing grinding habits, while stress management addresses the underlying cause, offering long-term prevention. For instance, a 30-year-old professional experiencing work-related stress might pair a dentist-prescribed mouthguard with a nightly meditation routine. Over time, as stress levels decrease, reliance on the mouthguard may lessen, though its use remains advisable during particularly stressful periods. This dual strategy not only preserves gum health but also improves overall sleep quality, as grinding often disrupts rest.
In practice, integrating these measures requires commitment but yields tangible benefits. Start by scheduling a dental evaluation to assess grinding severity and obtain a custom mouthguard if needed. Concurrently, experiment with stress-reduction techniques—whether guided meditation apps, yoga, or journaling—to identify what works best for your lifestyle. For families, modeling these habits can instill good oral care practices in children, reducing their future risk. By combining proactive protection with behavioral change, individuals can effectively minimize gum recession and safeguard their oral health for years to come.
Frequently asked questions
Yes, grinding teeth (bruxism) can directly contribute to gum recession. The excessive force from grinding can damage the gum tissue and the bone supporting the teeth, leading to recession over time.
Teeth grinding places abnormal pressure on the teeth and gums, causing inflammation and wear. This can weaken the gum tissue, making it more susceptible to receding as the supporting structures are compromised.
Gum recession is generally not reversible, but its progression can be halted. Treatment for bruxism, such as wearing a night guard, can prevent further damage, and gum grafting may be considered to restore lost tissue.
Yes, other factors like poor oral hygiene, periodontal disease, aggressive brushing, and genetic predisposition can also cause gum recession. Grinding exacerbates these issues by increasing stress on the gums.
To prevent gum recession from grinding, use a custom-fitted night guard to reduce pressure on the teeth and gums. Additionally, maintain good oral hygiene, address stress (a common cause of bruxism), and visit your dentist regularly for check-ups.