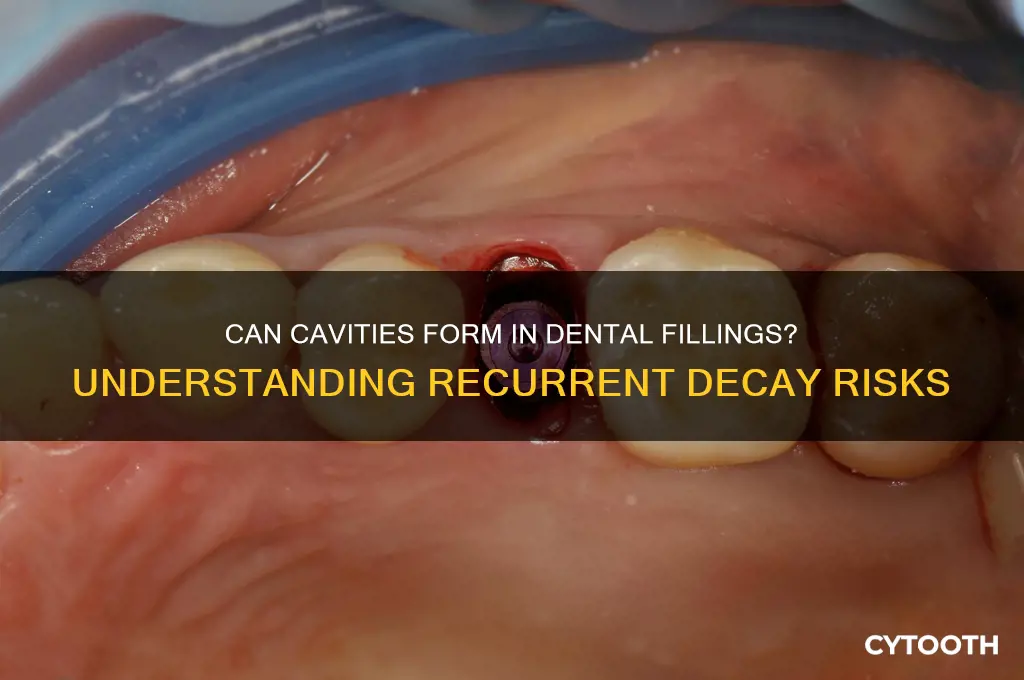
Many people wonder if it’s possible to develop cavities in or around existing dental fillings, a concern that highlights the complexities of oral health. While fillings are designed to restore damaged teeth and prevent further decay, they are not entirely immune to future issues. Over time, factors such as poor oral hygiene, wear and tear, or gaps between the filling and the tooth can create opportunities for bacteria to infiltrate and cause new decay. This raises the question of whether cavities can form directly in fillings or if they develop in the surrounding tooth structure, emphasizing the importance of regular dental check-ups and proper care to maintain the longevity of dental restorations.
| Characteristics | Values |
|---|---|
| Can cavities form in existing fillings? | Yes, cavities can form around or under fillings, especially if the filling is damaged, worn, or poorly sealed. |
| Common causes | Poor oral hygiene, recurrent decay, acidic diet, dry mouth, or faulty fillings. |
| Types of fillings affected | All types (amalgam, composite, ceramic, gold) can be susceptible. |
| Symptoms | Tooth sensitivity, pain, visible discoloration, or rough edges around the filling. |
| Prevention | Regular dental check-ups, good oral hygiene, fluoride use, and avoiding sugary/acidic foods. |
| Treatment | Replacement or repair of the filling, root canal (if decay reaches the pulp), or extraction in severe cases. |
| Risk factors | Poor oral care, frequent snacking, dry mouth conditions, or existing dental issues. |
| Frequency | Common, especially in older fillings or those with improper placement. |
| Latest research (as of 2023) | Advances in adhesive dentistry and materials aim to reduce recurrent decay under fillings. |
What You'll Learn

Can decay occur under fillings?
Dental fillings are designed to restore teeth damaged by decay, but they aren’t invincible. Over time, the margin where the filling meets the tooth can weaken, creating a microscopic gap. This gap becomes a breeding ground for bacteria, which thrive in the hard-to-reach space between the filling and the tooth. As these bacteria feed on sugars and starches, they produce acids that erode the tooth structure, leading to recurrent decay. This process is insidious because it often occurs without noticeable symptoms until the damage is significant.
Preventing decay under fillings requires vigilance and proactive care. Brush twice daily with fluoride toothpaste, ensuring you clean around the edges of fillings where plaque can accumulate. Floss daily to remove debris from between teeth and along the gumline, areas prone to recurrent decay. Limit sugary and acidic foods, as these accelerate enamel erosion. Regular dental check-ups are critical—dentists use tools like X-rays to detect early signs of decay beneath fillings, often before symptoms appear. Addressing issues early can prevent the need for more invasive treatments like root canals or crown replacements.
Comparing fillings, amalgam (metal) and composite (tooth-colored) fillings have different lifespans and risks. Amalgam fillings typically last 10–15 years but can corrode or expand, potentially weakening the tooth structure. Composite fillings, while aesthetically pleasing, are more prone to wear and chipping, increasing the risk of gaps forming. Regardless of material, all fillings eventually degrade, making them susceptible to recurrent decay. Patients should discuss their options with their dentist, weighing factors like durability, cost, and appearance to choose the best fit for their needs.
A practical tip for monitoring fillings is to pay attention to subtle changes. Sensitivity to hot, cold, or sweet foods, mild pain when biting, or visible discoloration around the filling can signal trouble. If you notice any of these symptoms, schedule a dental appointment immediately. Early intervention can often save the tooth and prevent the need for a complete filling replacement. Additionally, using antimicrobial mouthwash can reduce bacterial buildup, though it’s not a substitute for proper brushing and flossing. By staying proactive, you can extend the life of your fillings and protect your teeth from further decay.
Invisalign with a Missing Tooth: Is It Possible? Find Out!
You may want to see also

Signs of cavities around fillings
Dental fillings, while effective at restoring damaged teeth, are not impervious to further decay. Over time, the margins where the filling meets the tooth can weaken, creating opportunities for bacteria to infiltrate and cause new cavities. Recognizing the early signs of decay around fillings is crucial for prompt intervention and prevention of more extensive damage.
One of the most noticeable indicators is sensitivity to temperature or sweets. If you experience a sharp, sudden pain when consuming hot, cold, or sugary foods, it may signal that decay is present around the filling. This sensitivity often arises because the protective enamel has been compromised, exposing the underlying dentin and nerves. Unlike general tooth sensitivity, this discomfort is typically localized to the area around the filling.
Another telltale sign is visible discoloration or staining near the filling. While fillings themselves can darken over time, new dark spots or white chalky areas on the tooth surface around the restoration often indicate mineral loss and early decay. Regularly inspecting your teeth in a well-lit mirror can help you spot these changes early. If you notice any unusual discoloration, consult your dentist promptly.
Pain or discomfort when biting down is another red flag. If you feel pressure or pain around a filled tooth while chewing, it could mean that decay has progressed enough to weaken the tooth structure. In some cases, recurrent decay can cause the filling to become loose or even fall out, leaving the tooth vulnerable to further damage.
To prevent cavities around fillings, maintain excellent oral hygiene by brushing twice daily with fluoride toothpaste, flossing daily, and using an antimicrobial mouthwash. Schedule regular dental check-ups every six months, or more frequently if you’re at higher risk for decay. Your dentist may recommend dental sealants or fluoride treatments to strengthen the tooth enamel around fillings. Early detection and treatment are key to preserving the longevity of your dental restorations and overall oral health.
Smoking Weed Post-Tooth Filling: Risks and Recovery Tips
You may want to see also

Preventing cavities in filled teeth
Filled teeth are not immune to cavities. Despite the protective barrier a filling provides, the margins where the filling meets the tooth are vulnerable to bacterial infiltration. Over time, plaque can accumulate in these areas, leading to decay around the edges of the filling—a condition known as recurrent decay. This highlights the importance of proactive care to safeguard filled teeth from further damage.
One of the most effective strategies for preventing cavities in filled teeth is maintaining impeccable oral hygiene. Brush twice daily with a fluoride toothpaste, ensuring you clean all surfaces of the teeth, including around the fillings. Flossing is equally critical, as it removes plaque and food particles from between teeth and along the gumline where fillings are often placed. For added protection, incorporate an antimicrobial mouthwash into your routine to reduce bacterial buildup. Consistency is key; irregular hygiene practices leave filled teeth susceptible to recurrent decay.
Dietary choices play a significant role in cavity prevention. Limit frequent consumption of sugary and acidic foods, as these create an environment conducive to bacterial growth and enamel erosion. Instead, opt for tooth-friendly snacks like crunchy vegetables, cheese, or nuts, which stimulate saliva production and help neutralize acids. Drinking water throughout the day, especially after meals, can also rinse away debris and dilute acids in the mouth. For those prone to cavities, reducing sugar intake is not just advice—it’s a necessity.
Regular dental check-ups are indispensable for monitoring the health of filled teeth. Dentists can detect early signs of recurrent decay, often invisible to the naked eye, and address them before they worsen. Professional cleanings remove hardened plaque (tartar) that brushing alone cannot eliminate, further reducing the risk of cavities. Depending on your susceptibility to decay, your dentist may recommend additional preventive measures, such as fluoride treatments or dental sealants, to fortify vulnerable areas.
Lastly, consider the longevity of your fillings. Most fillings have a finite lifespan, typically 5–15 years, depending on the material and wear. Over time, fillings can crack, chip, or become loose, creating gaps where bacteria can thrive. If you notice sensitivity, pain, or visible damage around a filling, seek dental care promptly. Replacing or repairing compromised fillings is a proactive step to prevent cavities and preserve the integrity of the tooth. Ignoring these signs can lead to more extensive—and costly—dental work down the line.
Missing Tooth? Here’s How Braces Can Still Work for You
You may want to see also

Recurrent decay after fillings
Recurrent decay around fillings, often called secondary caries, is a frustrating reality for many patients. Despite the initial success of a filling, bacteria can infiltrate the tiny gap between the restoration and the tooth, leading to new decay. This occurs because fillings, while durable, aren't a perfect seal. Over time, factors like chewing forces, temperature changes, and natural wear can create microscopic spaces where bacteria thrive.
Sugary and acidic foods further fuel this process, providing the fuel for bacterial acid production that erodes enamel and attacks the vulnerable interface between tooth and filling.
Imagine a poorly sealed window. Even a small gap allows drafts and moisture to seep in, causing damage over time. Similarly, the margin where the filling meets the tooth is a critical area. If not meticulously prepared and sealed during the filling procedure, it becomes a breeding ground for decay-causing bacteria. This is why proper isolation techniques during the filling process are crucial. Dentists use rubber dams and other tools to keep the area dry and free from saliva and debris, ensuring a tight bond between the filling material and the tooth structure.
Inadequate isolation can lead to contamination, compromising the seal and increasing the risk of recurrent decay.
Preventing recurrent decay requires a multi-pronged approach. Firstly, meticulous oral hygiene is paramount. Brushing twice daily with fluoride toothpaste and flossing regularly removes plaque buildup, the primary culprit behind decay. Secondly, limiting sugary and acidic foods and beverages reduces the fuel source for bacteria. Regular dental checkups and cleanings are essential for early detection and removal of any early signs of decay around fillings. In some cases, dentists may recommend fluoride treatments or sealants to provide an extra layer of protection.
For high-risk individuals, more frequent checkups and preventive measures may be necessary.
While fillings are a common and effective solution for cavities, they aren't a permanent fix. Understanding the risk of recurrent decay and taking proactive steps to maintain good oral hygiene and dietary habits are crucial for preserving the longevity of fillings and overall dental health. Remember, prevention is always better than cure, and a little extra care can go a long way in keeping your smile healthy and cavity-free.
Veneers with a Missing Tooth: What Are Your Options?
You may want to see also

Treatment for cavities in fillings
Recurrent decay around existing fillings is a common issue, often stemming from marginal leakage where the filling meets the tooth. This creates a microscopic gap that traps bacteria and debris, leading to new decay. Treatment for cavities in fillings requires a precise, multi-step approach to address both the existing restoration and the new decay.
Assessment and Removal: The first step involves a thorough examination using radiographs and visual inspection to determine the extent of the decay. If the cavity is detected early, the dentist may only need to remove the compromised portion of the filling and the surrounding decayed tooth structure. For more extensive cases, the entire filling might need to be extracted, especially if it’s an older amalgam or composite restoration that has deteriorated over time.
Prevention of Further Damage: Once the decay is removed, the dentist will clean the area to eliminate bacteria and debris. In some cases, a dental dam may be used to isolate the tooth and prevent contamination during the procedure. If the decay has reached the dentin layer, a liner or base material, such as calcium hydroxide or glass ionomer, may be applied to protect the pulp and seal the tooth against sensitivity.
Restoration Options: The choice of restoration depends on the size and location of the cavity. For small lesions, a composite resin filling may suffice, offering aesthetic benefits and adequate strength. Larger cavities, especially in load-bearing areas like molars, may require an inlay, onlay, or crown to restore function and prevent fracture. Modern materials like ceramic or zirconia crowns provide durability and natural appearance, though they come at a higher cost compared to traditional amalgam fillings.
Post-Treatment Care: After the new restoration is placed, patients should follow specific care instructions to ensure longevity. Avoid chewing hard foods for 24–48 hours, especially with composite fillings that require time to fully cure. Maintain excellent oral hygiene, including twice-daily brushing with fluoride toothpaste and daily flossing. Regular dental check-ups every six months are essential to monitor the restoration and detect any early signs of recurrent decay.
Long-Term Considerations: While treating cavities in fillings is effective, prevention remains key. Reducing sugar intake, using antimicrobial mouthwash, and applying fluoride treatments can minimize the risk of future decay. For patients prone to recurrent cavities, sealants or prescription-strength fluoride products may be recommended. Addressing the underlying causes, such as dry mouth or poor oral hygiene, is crucial to breaking the cycle of recurrent decay.
Does a Dental Crown Hurt? What to Expect During the Procedure
You may want to see also
Frequently asked questions
Yes, it is possible to develop cavities around or under existing fillings, especially if the filling is old, damaged, or poorly sealed, allowing bacteria to accumulate.
Cavities can form if bacteria and plaque build up along the edges of a filling or if the filling becomes loose or cracked, creating gaps where decay can start.
Yes, cavities under fillings may not cause noticeable symptoms initially, but they can be detected during dental exams or X-rays before they progress.
Maintain good oral hygiene by brushing twice daily, flossing regularly, and visiting your dentist for check-ups. Avoid sugary foods and ensure fillings are inspected and replaced if damaged.