Root canal treatment is a common dental procedure designed to save a severely damaged or infected tooth by removing the infected pulp and sealing the tooth. While this process effectively eliminates the risk of further infection, many patients wonder if a root canal-treated tooth can still develop a cavity. The answer is yes—although the nerve and pulp are removed, the remaining tooth structure is still susceptible to decay, especially if proper oral hygiene is not maintained. Factors such as poor brushing, frequent sugar consumption, or a lack of regular dental check-ups can contribute to the formation of cavities on a root canal-treated tooth. Additionally, the crown or filling placed after the procedure can sometimes wear down or develop gaps, exposing the tooth to bacteria and increasing the risk of decay. Therefore, it is crucial to continue practicing good oral care and visiting your dentist regularly to ensure the longevity of a root canal-treated tooth.
| Characteristics | Values |
|---|---|
| Can a root canal tooth get a cavity? | Yes, but it is rare. Root canal-treated teeth are less susceptible to decay due to the removal of the pulp and nerve, but the remaining crown structure can still decay. |
| Reasons for decay in a root canal tooth | 1. Decay in the remaining tooth structure above the gum line. 2. Poor oral hygiene. 3. Inadequate restoration (e.g., faulty crown or filling). 4. Secondary decay around the restoration margin. |
| Prevention | 1. Maintain good oral hygiene (brushing, flossing). 2. Regular dental check-ups. 3. Proper restoration with a crown or filling. 4. Avoid sugary and acidic foods. |
| Treatment | 1. Removal of decay and replacement of the restoration. 2. In severe cases, retreatment of the root canal or extraction may be necessary. |
| Risk Factors | 1. Poor oral hygiene. 2. Existing dental restorations with gaps or cracks. 3. Dry mouth (reduced saliva flow). 4. High sugar diet. |
| Longevity of a root canal tooth | With proper care, a root canal-treated tooth can last a lifetime, but decay can compromise its longevity. |
| Common Misconception | Many believe a root canal-treated tooth is immune to decay, but the crown portion can still be affected. |
What You'll Learn
- Root canal success rates: How effective are root canals in preventing further decay and cavities
- Secondary infections: Can bacteria re-enter a treated tooth and cause new cavities
- Crown protection: Does a dental crown prevent cavities in a root canal tooth
- Restoration quality: How does the quality of filling material impact cavity risk
- Oral hygiene post-treatment: Does poor care after a root canal increase cavity chances

Root canal success rates: How effective are root canals in preventing further decay and cavities?
Root canals are a common dental procedure designed to save a severely damaged or infected tooth by removing the pulp, cleaning the canal, and sealing it to prevent further infection. But how effective are they in preventing further decay and cavities? The success rate of root canals is impressively high, typically ranging between 85% and 97%, depending on factors like the tooth's location, the skill of the dentist, and the patient's oral hygiene practices. This means that in the vast majority of cases, a root canal effectively stops the progression of decay and eliminates the risk of cavities in the treated tooth. However, it’s crucial to understand that while the internal structure is protected, the outer crown of the tooth remains vulnerable to decay, especially if not properly cared for.
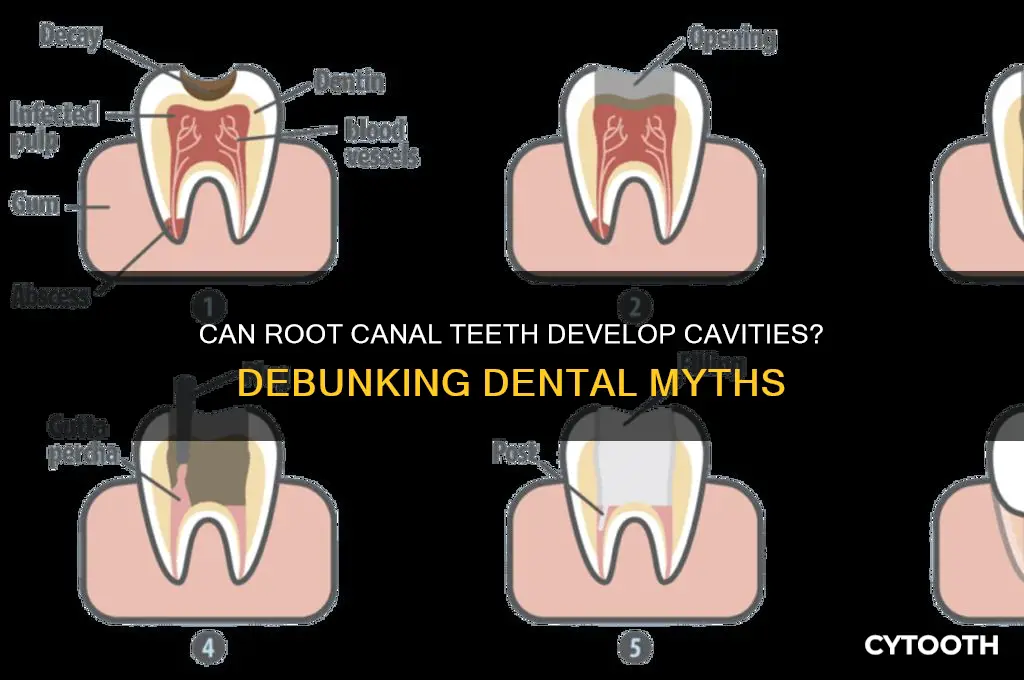
One of the key reasons root canals are so effective is their ability to eliminate the source of infection—the dental pulp. Once the pulp is removed and the canal is sealed with a biocompatible material like gutta-percha, bacteria cannot re-enter the tooth's interior. This prevents further decay from spreading internally. However, the treated tooth is still susceptible to external factors, such as plaque buildup and poor oral hygiene, which can lead to cavities on the remaining tooth structure. For instance, a tooth that has undergone a root canal often requires a dental crown to protect it from fractures and decay, as the absence of pulp can make the tooth more brittle over time.
Comparatively, untreated infected teeth have a near 100% chance of worsening decay, abscess formation, and eventual tooth loss. Root canals, therefore, are not just effective but essential in halting this progression. Studies show that teeth treated with root canals can last a lifetime if properly maintained. This includes regular brushing, flossing, and dental check-ups, as well as addressing issues like dry mouth or grinding, which can increase the risk of decay. Patients should also be aware that while the treated tooth itself cannot develop a new cavity internally, the area around the crown margin or exposed roots can still decay if neglected.
To maximize the success of a root canal and prevent cavities, patients should follow specific post-treatment care instructions. This includes avoiding hard or sticky foods immediately after the procedure, maintaining a low-sugar diet, and using fluoride toothpaste to strengthen the remaining tooth structure. For individuals with a history of frequent cavities, dentists may recommend additional preventive measures, such as fluoride treatments or dental sealants. Ultimately, while root canals are highly effective in preventing further internal decay, their long-term success relies heavily on the patient’s commitment to oral hygiene and regular dental care.
Veneers with a Missing Tooth: What Are Your Options?
You may want to see also

Secondary infections: Can bacteria re-enter a treated tooth and cause new cavities?
Root canal treatment aims to eliminate infection by removing the tooth's pulp, cleaning the canals, and sealing them to prevent bacterial re-entry. However, secondary infections can occur if bacteria find a way back into the treated tooth. This typically happens through cracks in the restoration, poorly fitting crowns, or new decay around the margins of fillings or crowns. For instance, a study in the *Journal of Endodontics* found that 12% of root canal-treated teeth developed secondary infections due to inadequate coronal seals. These breaches allow oral bacteria to infiltrate the previously treated area, leading to recurrent decay or reinfection.
To minimize the risk of secondary infections, follow these steps after a root canal: ensure your dentist places a permanent crown within 3–4 weeks of the procedure, as temporary fillings are not airtight and can allow bacteria to seep in. Maintain impeccable oral hygiene by brushing twice daily with fluoride toothpaste and flossing daily, paying extra attention to the treated tooth. Avoid hard or sticky foods that could damage the restoration. Regular dental check-ups every six months are crucial for early detection of issues like cracks or decay around the restoration. If you notice symptoms like persistent pain, swelling, or sensitivity in a root canal-treated tooth, seek immediate dental care, as these could indicate a secondary infection.
Comparatively, while root canal-treated teeth are more susceptible to fractures due to the removal of the nerve and blood supply, they are not inherently more prone to cavities than vital teeth. The key difference lies in the restoration’s integrity. A vital tooth has natural defenses, such as saliva and enamel, to combat bacteria, whereas a root canal-treated tooth relies entirely on the quality of the filling or crown. For example, a study in *Clinical Oral Investigations* showed that 85% of secondary infections in root canal-treated teeth were associated with faulty restorations, compared to only 15% linked to new decay. This highlights the importance of precise dental work and patient vigilance.
Persuasively, investing in a high-quality crown and adhering to post-treatment care guidelines is not just a recommendation—it’s a necessity. A well-fitted crown acts as a barrier, preventing bacteria from re-entering the tooth and causing recurrent infections. For patients with a history of poor oral hygiene or multiple restorations, dentists may recommend additional preventive measures, such as antimicrobial mouth rinses or fluoride treatments. Ignoring these precautions can lead to costly and painful complications, including the need for retreatment or, in severe cases, extraction. By prioritizing preventive care, you can safeguard your treated tooth and avoid the pitfalls of secondary infections.
Pregnancy and Dental Care: Is It Safe to Fill a Tooth?
You may want to see also

Crown protection: Does a dental crown prevent cavities in a root canal tooth?
A dental crown, often recommended after a root canal, serves as a protective cap for the treated tooth. Its primary purpose is to restore strength, shape, and functionality, but does it also prevent cavities? The answer lies in understanding the nature of cavities and the role of a crown. Cavities occur when bacteria produce acids that erode enamel, but a root canal removes the tooth’s pulp, leaving behind non-living dentin. Since dentin is less susceptible to decay, the risk of cavities in a root canal tooth is significantly reduced. However, the crown itself acts as a barrier, shielding the remaining tooth structure from external factors like plaque and acids, further minimizing the risk.
Consider the anatomy of a crowned tooth post-root canal. The crown covers the entire visible portion of the tooth, eliminating crevices where bacteria might accumulate. This seamless coverage reduces the likelihood of plaque buildup, a primary contributor to cavities. Additionally, crowns are typically made of durable materials like porcelain or ceramic, which are resistant to decay. While the crowned tooth is less prone to cavities, it’s not entirely immune. The junction where the crown meets the gum line remains vulnerable, as this area can still harbor bacteria if oral hygiene is poor.
From a practical standpoint, maintaining oral hygiene is crucial even with a crown. Brush twice daily with fluoride toothpaste and floss regularly, paying special attention to the gum line around the crowned tooth. Dental check-ups every six months are essential for monitoring the crown’s integrity and ensuring no decay develops at the margins. For added protection, consider using antimicrobial mouthwash to reduce bacterial growth. While a crown provides robust protection, it’s not a substitute for diligent care.
Comparatively, a crowned root canal tooth has a lower cavity risk than a natural tooth, but it’s not zero. Unlike a natural tooth, the crowned tooth lacks living tissue, making it less susceptible to decay. However, the surrounding gum tissue and the crown’s margins require consistent care. In contrast, a natural tooth’s enamel is constantly at risk from acids and plaque. By understanding these differences, patients can take proactive steps to preserve their crowned tooth’s longevity.
In conclusion, a dental crown significantly reduces the risk of cavities in a root canal tooth by providing a protective barrier and eliminating vulnerable areas for bacteria. However, it’s not foolproof. Proper oral hygiene and regular dental visits are essential to ensure the crown remains effective. Think of the crown as a suit of armor—it protects the tooth, but the wearer must still maintain vigilance to avoid potential threats. With the right care, a crowned root canal tooth can remain cavity-free for years.
Pregnancy and Dental Care: Is Tooth Extraction Safe for Expecting Moms?
You may want to see also

Restoration quality: How does the quality of filling material impact cavity risk?
The quality of filling material used in a root canal-treated tooth plays a pivotal role in determining its susceptibility to secondary cavities. High-quality materials, such as composite resins or glass ionomers, create a tight seal that minimizes microleakage—the seepage of bacteria and fluids between the restoration and tooth structure. In contrast, subpar materials or improper placement can leave voids or gaps, providing entry points for bacteria to infiltrate and initiate decay. For instance, a study published in the *Journal of Endodontics* found that teeth restored with inferior materials had a 30% higher risk of recurrent caries within five years compared to those with premium restorations.
Consider the process of selecting filling materials as a critical step in cavity prevention. Composite resins, known for their durability and aesthetic appeal, are often recommended for visible areas, while amalgam fillings, though less common today, remain a robust option for molars due to their strength. Glass ionomers, which release fluoride over time, offer an added layer of protection by remineralizing enamel and inhibiting bacterial growth. However, their longevity is shorter, making them less ideal for high-stress areas. Dentists must weigh factors like patient age, bite force, and oral hygiene habits when choosing materials to optimize long-term success.
A persuasive argument for investing in high-quality restorations lies in their cost-effectiveness over time. While premium materials may carry a higher upfront cost, they reduce the likelihood of recurrent decay, which often necessitates more invasive and expensive treatments, such as re-treatment or extraction. For example, a root canal with a substandard filling might fail within three years, requiring a costly dental implant or bridge. Conversely, a well-executed restoration using top-tier materials can last a decade or more, saving both money and discomfort in the long run.
Comparatively, the impact of material quality becomes evident when examining real-world outcomes. Teeth restored with low-quality materials often exhibit marginal breakdown, where the interface between the filling and tooth deteriorates, allowing bacteria to penetrate. This is particularly problematic in root canal-treated teeth, which lack vitality and are more reliant on the integrity of the restoration for protection. In contrast, teeth with high-quality fillings maintain their structural integrity, significantly lowering the risk of secondary cavities. A longitudinal study in *Clinical Oral Investigations* highlighted that 85% of root canal teeth with premium restorations remained cavity-free after seven years, compared to just 55% of those with inferior fillings.
To minimize cavity risk in root canal-treated teeth, patients and practitioners should prioritize restoration quality. Practical tips include opting for materials with proven longevity, ensuring precise placement by an experienced dentist, and maintaining regular check-ups to monitor the integrity of the restoration. Additionally, practicing good oral hygiene—brushing twice daily with fluoride toothpaste, flossing, and using antimicrobial mouthwash—can further safeguard against decay. By combining high-quality materials with diligent care, the risk of cavities in root canal-treated teeth can be dramatically reduced, preserving oral health for years to come.

Oral hygiene post-treatment: Does poor care after a root canal increase cavity chances?
After a root canal, the treated tooth is more vulnerable than you might think. While the procedure removes infected pulp and seals the tooth, the restored structure—often a crown or filling—isn’t invincible. Poor oral hygiene post-treatment can lead to secondary decay, where bacteria infiltrate gaps or weakened areas around the restoration. This isn’t a new cavity in the traditional sense, since the nerve is gone, but it’s a serious issue that can compromise the tooth’s integrity. Think of it as a breach in the fortress; neglect leaves it open to attack.
Consider the mechanics: a root canal tooth relies heavily on its restoration to function. If plaque accumulates due to inadequate brushing or flossing, acids from bacteria can erode the margins of a crown or filling. Over time, this creates pathways for decay to reach the remaining tooth structure or even the root surface. For instance, a study in the *Journal of Endodontics* found that 20% of root canal failures were linked to recurrent decay, often tied to poor oral hygiene. This isn’t just about aesthetics—it can lead to reinfection, requiring re-treatment or extraction.
Here’s the actionable part: post-root canal care isn’t optional; it’s critical. Brush twice daily with a fluoride toothpaste, ensuring you clean around the restored tooth thoroughly. Floss daily, using tools like interdental brushes if space is tight. Visit your dentist every six months for check-ups and cleanings, as they can spot early signs of decay around restorations. Avoid sugary snacks and drinks, which fuel bacterial activity. If you’re prone to plaque buildup, consider an antimicrobial mouthwash prescribed by your dentist. These steps aren’t just recommendations—they’re your defense against a costly and painful setback.
Compare this to maintaining a car: after a major repair, you wouldn’t ignore routine maintenance. Similarly, a root canal tooth demands consistent care to avoid breakdown. Patients often assume the treated tooth is “dead” and immune to issues, but the surrounding tissues and restoration remain at risk. For example, a 45-year-old patient with a crowned root canal tooth might develop decay at the crown’s margin within 5 years if they skip flossing. This isn’t fate—it’s preventable with discipline and awareness.
In conclusion, poor oral hygiene post-root canal doesn’t just increase cavity chances; it invites disaster. The treated tooth’s survival depends on your vigilance. Treat it like a high-maintenance asset, not a forgotten corner of your mouth. Remember, the goal isn’t just to save the tooth once—it’s to keep it healthy for life.
Frequently asked questions
While rare, it is possible to get a cavity in a root canal tooth, especially if the restoration (crown or filling) is damaged or if decay occurs in the remaining tooth structure above the gum line.
A cavity can form if the tooth’s restoration (crown or filling) is compromised, allowing bacteria to re-enter the tooth or affect the surrounding area, or if decay occurs in the remaining tooth structure.
Yes, the part of the tooth above the gum line still has enamel that can decay if proper oral hygiene is not maintained or if the restoration is damaged.
If the restoration is not properly sealed or becomes damaged, bacteria can re-enter the tooth, potentially causing new decay or re-infection, though this is uncommon with proper care.
Maintain good oral hygiene, attend regular dental check-ups, ensure the restoration is intact, and avoid habits like teeth grinding that can damage the tooth or restoration.














