Gum grafts are a surgical procedure often recommended to address gum recession, a condition where the gum tissue pulls away from the tooth, exposing the root. While not always necessary, gum grafts can be crucial for preventing further recession, reducing tooth sensitivity, and protecting against potential tooth loss. The necessity of a gum graft depends on the severity of the recession, the patient’s oral health, and their symptoms. Dentists typically evaluate factors such as tooth mobility, bone loss, and the patient’s aesthetic concerns before recommending the procedure. For mild cases, non-surgical treatments like improved oral hygiene or antimicrobial mouthwashes may suffice, but more advanced recession often requires a graft to restore gum health and function.
| Characteristics | Values |
|---|---|
| Purpose | To treat gum recession, protect tooth roots, and improve aesthetics. |
| Necessity | Depends on severity of gum recession and associated symptoms. |
| Common Reasons | Tooth sensitivity, root decay, aesthetic concerns, and risk of tooth loss. |
| Types of Gum Grafts | Connective tissue graft, free gingival graft, pedicle graft, Allograft. |
| Success Rate | High, typically 90-95% with proper care. |
| Recovery Time | 1-2 weeks for initial healing; full recovery may take 3-6 months. |
| Cost | $600 to $3,000 per graft, depending on complexity and location. |
| Alternatives | Non-surgical treatments like deep cleaning, fluoride application, or enamel bonding (for mild cases). |
| Long-Term Benefits | Prevents further recession, reduces sensitivity, and improves oral health. |
| Risks/Complications | Infection, bleeding, graft failure, or temporary discomfort. |
| Patient Suitability | Recommended for patients with significant gum recession or related issues. |
| Maintenance | Good oral hygiene and regular dental check-ups are essential post-surgery. |
| Aesthetic Improvement | Enhances smile appearance by covering exposed roots. |
| Insurance Coverage | Often partially covered if deemed medically necessary. |
| Prevention | Proper brushing, flossing, and avoiding aggressive dental habits can reduce the need for gum grafts. |
What You'll Learn
- Receding Gums Causes: Poor oral hygiene, genetics, aggressive brushing, or periodontal disease lead to gum recession
- Gum Graft Benefits: Protects roots, reduces sensitivity, improves aesthetics, and prevents further tissue loss
- Alternatives to Grafts: Non-surgical options like deep cleaning, antibiotics, or enamel bonding in mild cases
- Surgical Procedure Types: Connective tissue, free gingival, or pedicle grafts depending on recession severity
- Recovery and Aftercare: Post-surgery care includes pain management, soft diet, and proper oral hygiene

Receding Gums Causes: Poor oral hygiene, genetics, aggressive brushing, or periodontal disease lead to gum recession
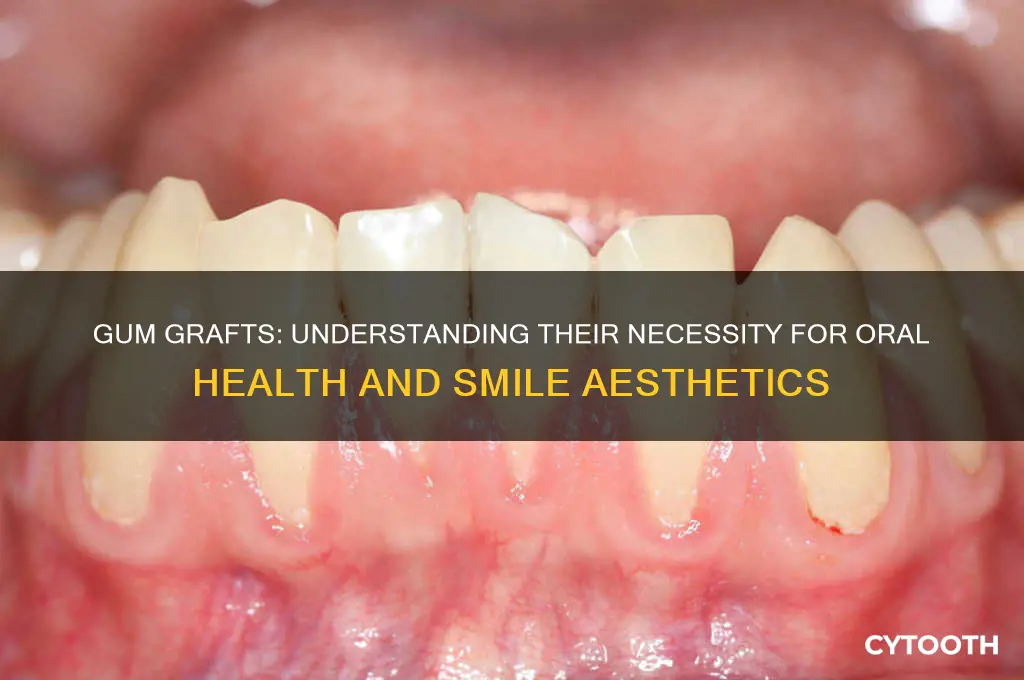
Gum recession is a gradual process where the margin of the gum tissue surrounding the teeth wears away, or pulls back, exposing more of the tooth, and in severe cases, the tooth's root. This condition is not merely a cosmetic concern; it can lead to increased sensitivity, tooth decay, and even tooth loss if left untreated. Understanding the causes of receding gums is the first step in determining whether interventions like gum grafts are necessary.
Poor oral hygiene stands as a primary culprit behind gum recession. When plaque and tartar build up along the gum line, they create a breeding ground for bacteria, leading to inflammation and infection known as gingivitis. If untreated, this progresses to periodontitis, a severe gum infection that damages the soft tissue and bone supporting the teeth. To combat this, dentists recommend brushing twice a day with a fluoride toothpaste, flossing daily, and using an antimicrobial mouthwash. For those with early signs of gum recession, a soft-bristled toothbrush and gentle brushing technique are essential. Avoid vigorous scrubbing, as it can exacerbate the problem.
Genetics play a significant role in determining an individual's susceptibility to gum recession. Studies suggest that up to 30% of the population may be predisposed to gum disease, regardless of their oral hygiene habits. If your parents or siblings have experienced gum recession, you are at a higher risk. While genetic factors cannot be altered, awareness of this predisposition can prompt more vigilant oral care and regular dental check-ups. Dentists may recommend more frequent cleanings or specialized treatments for those with a family history of gum issues.
Aggressive brushing is a common yet often overlooked cause of receding gums. Brushing too hard or using a hard-bristled toothbrush can wear away the delicate gum tissue over time. This mechanical trauma can lead to gum recession, especially in individuals who brush horizontally rather than using the recommended 45-degree angle. Dentists advise using a soft-bristled toothbrush and adopting the Bass brushing technique, which involves gentle, circular motions. Electric toothbrushes with pressure sensors can also help prevent overzealous brushing.
Periodontal disease, a severe infection of the gums, is a leading cause of gum recession in adults. This condition occurs when plaque buildup leads to inflammation and infection, causing the gums to pull away from the teeth. Advanced periodontal disease can destroy the bone and connective tissue holding teeth in place, leading to tooth loss. Treatment often involves deep cleaning procedures like scaling and root planing to remove plaque and tartar below the gum line. In severe cases, surgical interventions such as flap surgery or bone grafts may be necessary to repair the damage.
In conclusion, receding gums can result from a combination of factors, including poor oral hygiene, genetic predisposition, aggressive brushing, and periodontal disease. While some causes, like genetics, are beyond our control, others can be mitigated through proper oral care and regular dental visits. Recognizing the early signs of gum recession—such as tooth sensitivity, bleeding gums, or visible roots—can prompt timely intervention. For those with advanced gum recession, gum grafts may be necessary to restore gum tissue, reduce sensitivity, and prevent further damage. Consulting with a periodontist can provide personalized treatment options tailored to the severity and underlying causes of your condition.

Gum Graft Benefits: Protects roots, reduces sensitivity, improves aesthetics, and prevents further tissue loss
Gum recession, often caused by periodontal disease, aggressive brushing, or genetic factors, exposes tooth roots, leading to sensitivity, decay, and aesthetic concerns. Gum grafts address these issues by covering exposed roots with healthy tissue, creating a protective barrier against further damage. This procedure is not merely cosmetic; it’s a functional intervention that halts the progression of oral health problems. For instance, exposed roots are more susceptible to cavities because they lack the protective enamel layer found on the crown of the tooth. By covering these areas, gum grafts reduce the risk of root decay, which is harder to treat and more costly to repair than typical cavities.
Consider the daily discomfort of tooth sensitivity—a sharp pain when sipping hot coffee or biting into ice cream. This sensitivity arises when dentin, the layer beneath enamel, is exposed. Gum grafts alleviate this by regenerating the gumline, effectively shielding the dentin and reducing nerve exposure. Patients often report significant relief within weeks of the procedure, allowing them to enjoy their favorite foods without wincing. For those with severe sensitivity, this benefit alone can justify the decision to undergo a gum graft, as over-the-counter desensitizing toothpastes often provide only temporary relief.
Aesthetically, receding gums create the illusion of longer teeth, often described as a "toothy" smile, which many find unattractive. Gum grafts restore the natural gum-to-tooth ratio, enhancing the smile’s symmetry and balance. This improvement is particularly noticeable in the front teeth, where cosmetic concerns are most visible. Techniques like the connective tissue graft or the pedicle graft are tailored to individual needs, ensuring both functional and visual success. For patients self-conscious about their smile, this transformation can boost confidence and improve quality of life.
Perhaps the most critical benefit of gum grafts is their ability to prevent further tissue loss. Left untreated, gum recession can lead to tooth mobility and eventual tooth loss as the supporting structures weaken. By stabilizing the gumline, grafts preserve the periodontal attachment, the fibers that anchor teeth to the bone. This is especially vital for older adults or those with advanced periodontal disease, as it slows the progression of oral deterioration. Think of it as reinforcing a foundation before a house begins to crumble—proactive care that avoids more extensive (and expensive) interventions later.
Finally, while gum grafts offer substantial benefits, they require careful consideration. Post-operative care is crucial; patients must follow instructions diligently, such as avoiding hard or crunchy foods for 2–3 weeks and maintaining impeccable oral hygiene. The procedure itself is typically performed under local anesthesia and takes about 1–2 hours, depending on the extent of the graft. Recovery varies, but most patients return to normal activities within a few days. For those weighing the necessity of a gum graft, the long-term advantages—root protection, reduced sensitivity, aesthetic enhancement, and tissue preservation—often outweigh the temporary inconveniences of the procedure.

Alternatives to Grafts: Non-surgical options like deep cleaning, antibiotics, or enamel bonding in mild cases
Gum recession, though common, doesn’t always require the invasiveness of a graft. In mild cases, where the exposure is minimal and symptoms like sensitivity are manageable, non-surgical interventions can halt progression and restore function. Deep cleaning, for instance, targets the root cause—bacterial buildup—by removing plaque and tartar below the gumline. This procedure, known as scaling and root planing, smooths the tooth root to discourage further bacterial adhesion. For adults over 30 with early-stage recession linked to gingivitis, this can be a first-line defense, often paired with a 0.12% chlorhexidine mouthwash for 30 days to reduce inflammation.
When infection is the culprit, antibiotics become a critical tool. A 7-day course of 500mg amoxicillin twice daily (or 500mg metronidazole for penicillin-allergic patients) can eliminate bacteria driving gum tissue loss. This is particularly effective in cases where deep pockets around the teeth harbor anaerobic bacteria. However, antibiotics alone are insufficient; they must accompany mechanical debridement to remove the biofilm where these pathogens thrive. For best results, patients should avoid smoking and maintain meticulous oral hygiene post-treatment.
Enamel bonding offers a cosmetic solution for mild recession, particularly when root exposure causes aesthetic concerns or heightened sensitivity. This procedure involves applying a tooth-colored composite resin to cover the exposed root surface, which is then hardened with a curing light. While not a cure for the underlying issue, bonding can provide immediate relief from sensitivity and improve appearance. It’s ideal for young adults or those with minimal recession (less than 2mm) who seek a quick, reversible option. However, bonding requires replacement every 5–7 years due to wear, making it a temporary fix compared to grafts.
Each of these alternatives has limitations. Deep cleaning and antibiotics address infection but won’t regenerate lost tissue. Enamel bonding masks the problem without treating it. Thus, they’re best suited for mild cases or as interim measures. Patients must weigh the convenience of non-surgical options against the long-term stability of grafts, consulting a periodontist to determine the most appropriate path based on recession severity, bone health, and personal priorities.

Surgical Procedure Types: Connective tissue, free gingival, or pedicle grafts depending on recession severity
Gum recession, if left untreated, can lead to tooth sensitivity, decay, and even tooth loss. When non-surgical methods fail to address the issue, gum grafts become a necessary intervention. The choice of surgical procedure—connective tissue, free gingival, or pedicle grafts—depends largely on the severity and location of the recession. Each technique offers distinct advantages and is tailored to specific clinical scenarios, ensuring optimal outcomes for patients.
Connective Tissue Grafts are the gold standard for treating single, isolated recessions or those with thin gum tissue. In this procedure, a small flap of tissue is harvested from the palate, and the underlying connective tissue is removed. This tissue is then sutured over the recessed area, providing a robust foundation for new gum growth. Patients typically experience minimal discomfort post-surgery, with healing times ranging from 1 to 2 weeks. This method is particularly effective for Miller Class I and II recessions, where the bone support is adequate, and the primary concern is soft tissue deficiency.
For patients with multiple adjacent recessions or insufficient tissue volume, Free Gingival Grafts may be more appropriate. This technique involves harvesting a thin layer of tissue directly from the palate, including the epithelium, and suturing it onto the recipient site. While it can result in a faster coverage of the exposed root, it often leaves a paler, less aesthetically pleasing appearance compared to connective tissue grafts. Recovery can be slightly more uncomfortable due to the palatal donor site, but it remains a viable option for cases requiring bulkier tissue augmentation.
Pedicle Grafts, on the other hand, utilize tissue from adjacent areas of the mouth, eliminating the need for a second surgical site. The most common type is the lateral pedicle graft, where tissue is rotated from a neighboring area to cover the recession. This method is ideal for patients with sufficient adjacent gum tissue and is particularly effective for treating recessions in the front teeth. However, it is limited by the availability of nearby tissue and may not be suitable for posterior teeth or extensive recessions.
Choosing the right graft type requires a thorough assessment of the patient’s oral health, the extent of recession, and aesthetic considerations. For instance, younger patients or those with high smile lines may prioritize the natural appearance achieved with connective tissue grafts, while older patients might opt for the simplicity of a pedicle graft. Regardless of the method, early intervention is key to preventing further complications. Post-operative care, including proper oral hygiene and avoiding smoking, significantly impacts the success of the procedure. By understanding these surgical options, patients and clinicians can make informed decisions to restore gum health effectively.

Recovery and Aftercare: Post-surgery care includes pain management, soft diet, and proper oral hygiene
Post-gum graft surgery, the first 48 hours are critical for healing. Pain management is paramount during this period. Over-the-counter medications like ibuprofen (600–800 mg every 6–8 hours) or acetaminophen (500–1000 mg every 4–6 hours) can alleviate discomfort, but avoid aspirin, as it may increase bleeding. For severe pain, your dentist might prescribe stronger analgesics. Applying an ice pack to the cheek in 20-minute intervals during the first 24 hours reduces swelling and numbs the area, providing additional relief.
Dietary adjustments are equally essential to protect the graft site. Stick to a soft, lukewarm diet for at least a week. Think smoothies, yogurt, mashed potatoes, and well-cooked soups. Avoid hot foods and beverages, as they can dissolve blood clots and delay healing. Crunchy, spicy, or acidic foods should also be avoided, as they can irritate the surgical site. Hydration is key, but use a straw to minimize contact with the graft area.
Oral hygiene must be meticulous yet gentle. For the first 24 hours, avoid rinsing or spitting forcefully to prevent dislodging the graft. After this initial period, rinse with a warm saltwater solution (1/2 teaspoon of salt in 8 ounces of water) 3–4 times daily to keep the area clean. Brush your teeth carefully, avoiding the graft site, and use a soft-bristled toothbrush. Your dentist may recommend a chlorhexidine mouthwash to reduce bacterial buildup, but follow their instructions closely, as overuse can stain teeth.
Long-term aftercare involves monitoring the graft site for signs of infection, such as persistent pain, pus, or fever. Attend all follow-up appointments to ensure proper healing. Gradually reintroduce firmer foods as tolerated, but avoid aggressive chewing near the graft for several weeks. Smoking and alcohol consumption should be avoided entirely, as they impair healing and increase the risk of graft failure. With diligent care, most patients experience a smooth recovery and improved gum health.
Frequently asked questions
Gum grafts are not always necessary for receding gums. Mild cases may be managed with improved oral hygiene, deep cleaning (scaling and root planing), or antimicrobial treatments. However, if gum recession is severe, causing sensitivity, root exposure, or risk of tooth loss, a gum graft may be recommended to restore gum tissue and protect the teeth.
You may need a gum graft if you experience symptoms like tooth sensitivity, visible tooth roots, gum line recession, or gum tissue loss. A dentist or periodontist will evaluate your condition through a clinical exam, X-rays, and discussion of your symptoms to determine if a gum graft is necessary.
No, gum grafts are not solely for cosmetic purposes. While they can improve the appearance of receding gums, they primarily serve a functional purpose. Gum grafts protect exposed tooth roots from decay, reduce sensitivity, prevent further gum recession, and help maintain overall oral health.














